Website Cases:
Additional case (NOT assigned):
Gross specimen videos:
| Organ |
Diagnosis |
Video |
| Aorta |
Aortic Dissection |
Video |
| Aorta |
Ball and Cage Artificial Heart Valve |
Video |
| Heart |
Coronary Artery Bypass Graft |
Video |
| Heart |
Dilated Cardiomyopathy |
Video |
| Heart |
Left Ventricular Hypertrophy |
Video |
| Heart |
Myocardial Infarction |
Video |
| Heart |
Rheumatic Heart Disease |
Video |
| Aorta |
Saccular Aneurysm |
Video |
CASE NUMBER 545
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 37-year-old man presented to the Emergency Department with a 1-month history of fatigue and a two-week history of a “rash”. He was from Botswana, visiting family in the United States, and noticed multiple lesions on his back. He was unmarried and frequently had sex with prostitutes. On physical examination, he was thin but otherwise in no apparent distress. The skin lesions were reddish purple in color, non-tender, and non-blanching to palpation. Several similar lesions were observed in the oropharynx. Laboratory findings were as follows:
TEST |
RESULT (reference range in parentheses) |
Hemoglobin |
10.2 gm/dL (11-13 gm/dL) |
Hct |
34.3% (35-44%) |
RDW |
13.2% (11.6-14.6%) |
MCV |
82 µm3 (80- 100 µm3) |
WBC |
3,200/mm3 (4500-11000 mm3) |
CBC Differential |
Neutrophils, 86% (normal 54-62%)
Monocytes, 8% (normal, 3-7%)
Lymphocytes, 6% (normal 25-33%) |
Platelets |
260,000/mm3 (150,000-400,000/mm3) |
Additional test results: The CD4 T cell count was 52 cells/mm3 (normal, 460-1600 cells/ mm3). Immunoassays were positive for HIV-1
Image Gallery:
Review Skin Histology
Norm No. 15 Skin
[DigitalScope]
Skin consists of keratinizing stratified squamous epithelium. The keratin layer is eosinophilic. Nuclei are not present. Beneath the keratin layer is a layer of flat epithelial cells with small pyknotic nuclei. Cells are regular and not crowded. These keratinocytes rest upon a layer of basal epithelium and a thin basement membrane. Beneath the epidermis is the dermis which consists of loose connective tissue. Within the dermis are sweat and sebaceous glands. Some slides contain hair follicles. There is no inflammation. The blood vessels are patent and do not contain thromboemboli.
|
Clinical Findings
There are multiple discrete violaceous plaques with a somewhat linear appearance that are more or less aligned along Langer (ie. cleavage lines). They are more or less symmetric. They may appear pink to brown and may be confluent or discrete and have a macular, papular or nodular appearance.
|
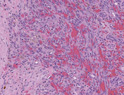
Microscopic Findings
There is an atypical spindle cell proliferation that appears as an ill-defined nodule in the subcutaneous tissue. Discrete blood vessel formation is not seen; however, there are slit-like spaces with abundant extravasated red blood cells and hemosiderin-laden macrophages. There is associated fibrosis and lymphocytes. No significant pleomorphism is seen. There is no necrosis or brisk mitotic activity.
|
Physical exam questions:
- Describe the lesions seen in the clinical image.
VM image questions:
- Describe the lesion in the virtual microscopy.
- What shape are the neoplastic cells?
- Is the lesion infiltrative or circumscribed?
- Is the epidermis involved?
- Is there necrosis?
- Is there brisk mitotic activity?
- Is the lesion pleomorphic or monomorphic?
Differential diagnosis questions:
545-1a. What is the differential diagnosis based on the initial clinical presentation?
545-1b.How do the laboratory values focus your differential diagnosis?
545-1c.What is the diagnosis based on the microscopic findings?
--ANSWER--
545-2. Which of the following best describes the expected clinical course for this patient, assuming his HIV is not treated?
- Tumors remain asymptomatic
- Tumors form nodules, involve lymph nodes and visceral organs
- Tumors extensively involve lymph nodes, 100% mortality within 3 years
- Tumors regress and reappear in other sites
- Tumors regress completely over time
--ANSWER--
545-3. Which of the following would be the most likely diagnosis in a 65-year-old man from Italy man who presented with similar skin lesions on his distal lower extremities?
- Angiosarcoma
- Bacillary angiomatosis
- Classic Kaposi sarcoma
- Epithelioid hemangioendothelioma
- Glomus tumor
--ANSWER--
545-4. Which of the following is the proposed mechanism for development of these tumors?
- Immune complex deposition stimulates vascular proliferation
- Increased HIF1-α production
- Increased VEGF production
- MYC amplification
- TP53 mutation
--ANSWER--
CASE NUMBER 11
(no virtual slide for this case)
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 5-day old infant girl is brought to the pediatrician when her mother notices that she turns bluish when crying or feeding. The pregnancy had no complications and the child was delivered by spontaneous vaginal delivery. Physical exam reveals a respiratory rate of 40 and 02 of 80% on room air. A right ventricular lift is palpated. S1 is normal, S2 is single and there is a harsh 3/6 systolic ejection murmur at the left upper sternal border.
Differential diagnosis questions:
11-1. What is the differential diagnosis?
--ANSWER--
Clinical History, part 2 (click here to open):
CASE NUMBER 195
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 65-year-old man who had been diagnosed with rheumatic heart disease when he was 35-years old presented to his primary care physician with a 3-month history of fever and chills and dyspnea. Physical exam revealed bilateral lower extremity pitting edema, a purpuric skin rash, and fingernail findings shown below. He was admitted to the hospital but died. Clinical and laboratory images and gross and microscopic images from the autopsy are provided.
Image Gallery:
|
Review Heart Histology
Slide 98HE
[DigitalScope]
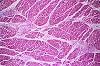
Normal heart tissue sections demonstrate no evidence of fibrosis or hemorrhage. Cardiac myocytes have moderately sized centrally located nuclei. Normal myocytes are not brightly eosinphilic. Normally no inflammation is seen. Normal cardiac myocytes do not show hypertrophy.
Locate the atrioventricular sulcus that contains a branch of the coronary arterial system (a muscular artery that exhibits moderate intimal thickening) embedded in the epicardial fat. Look at the connective tissue present between the ventricle and atrium. This is part of the cardiac skeleton into which cardiac muscle inserts. A leaflet of an A-V valve takes origin from the cardiac skeleton. Look at the atrial and ventricular endocardium, consisting of an endothelial lining and the underlying connective tissue (the endothelium is often stripped away during processing, but there are some areas where it has been preserved). With low power, locate the Purkinje fibers present immediately beneath the ventricular endocardium (note the appearance of these fibers in cross and longitudinal orientations). These conducting fibers are larger and paler staining than the cardiac muscle fibers. Note the meshwork arrangement of the cardiac muscle fibers in the myocardium.
|
Clinical Findings
Splinter hemorrhages were observed at digit tips. Blood cultures grew alpha-hemolytic streptococci. The alpha hemolysis on blood agar typical of Streptococcus viridans is shown. Gram stain shows gram positive cocci in chains.The heart weighed 400 grams. There was thickening of the mitral valve leaflets and the chordae tendineae. Many friable calcified pink-gray granular verrucae were present on the valve. In addition, a large vegetation of the same type was found on the left auricular endocardium.
|
Microscopic Findings
The section represents a portion of mitral valve, left atrium and left ventricle. The valve is greatly thickened and damaged. It is infiltrated with acute and chronic inflammatory cells, and shows a zone of necrosis and fibrosis in the central portion of the valve. The myocardium shows slight focal fibrosis, and focal acute inflammatory infiltration in some sections.
|
Physical exam questions:
- Describe the findings in the clinical image.
- What do you think is being shown here?
Gross image questions:
- Take a screenshot and identify the following on the gross image:
- the aortic valve
- lesional tissue
- left ventricle
- Where are the lesions originating? How would you describe them?
VM image questions:
- Take a screenshot and annotate:
- valvular tissue,
- an area of calcification, and
- an area of necrosis.
- Which type of inflammation do you think this is due to?
Differential diagnosis questions:
195-1a. What is the differential diagnosis?
195-1b. Based on the gross and microscopic findings, what is the correct diagnosis?
--ANSWER--
195-2. In this patient, which of the following is the most likely causative organism?
- Group A streptococcus
- Neisseria meningitidis
- Staphylococcus aureus
- Staphylococcus epidermidis
- Streptococcus viridans
--ANSWER--
195-3. Involvement of which of the following valves most suggestive of IV drug abuse?
- All valves are equally affected
- Aortic valve
- Mitral valve
- Pulmonic valve
- Tricuspid valve
--ANSWER--
CASE NUMBER 25
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 9-year-old girl from Cambodia who was visiting the United States was taken to the Emergency Department with recent onset dyspnea. She reported a 6-week history of painful, swollen joints. Physical exam revealed a temperature of 38C, cervical lymphadenopathy and pansystolic and diastolic murmurs. Laboratory analysis was positive for serum antibodies to streptolysin O. Although she was admitted to the hospital, she died of progressive heart failure. Gross and microscopic images of the autopsy are provided.
Image Gallery:
|
Review Heart Histology
Slide 98HE
[DigitalScope]
Normal heart tissue sections demonstrate no evidence of fibrosis or hemorrhage. Cardiac myocytes have moderately sized centrally located nuclei. Normal myocytes are not brightly eosinphilic. Normally no inflammation is seen. Normal cardiac myocytes do not show hypertrophy.
Locate the atrioventricular sulcus that contains a branch of the coronary arterial system (a muscular artery that exhibits moderate intimal thickening) embedded in the epicardial fat. Look at the connective tissue present between the ventricle and atrium. This is part of the cardiac skeleton into which cardiac muscle inserts. A leaflet of an A-V valve takes origin from the cardiac skeleton. Look at the atrial and ventricular endocardium, consisting of an endothelial lining and the underlying connective tissue (the endothelium is often stripped away during processing, but there are some areas where it has been preserved). With low power, locate the Purkinje fibers present immediately beneath the ventricular endocardium (note the appearance of these fibers in cross and longitudinal orientations). These conducting fibers are larger and paler staining than the cardiac muscle fibers. Note the meshwork arrangement of the cardiac muscle fibers in the myocardium.
|
Gross Findings
Her heart weighed 380 grams (normal for this age is about 115 grams). The pericardium was covered with a fibrinous exudate. The left ventricle was dilated and the myocardium was flabby. The mitral valve was slightly thickened as were the chordae tendineae. There was a MacCallum's patch in the left atrium. The liver weighed 780 grams (normal 750 grams). There was centrilobular congestion ("nutmeg liver").
|
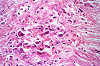
Microscopic Findings
The section includes the entire thickness of the myocardium and is taken through the mitral valve so that both left atrial and left ventricular myocardium are present in the section. The epicardium shows a prominent layer of fibrin on the surface; deep to this is young connective tissue with many capillaries, fibroblasts, and chronic inflammatory cells, i.e. granulation tissue. Thus, this is an organizing fibrinous pericarditis. There is also myocarditis present. The myocardial inflammation includes Aschoff bodies of different ages. Identify very early, intermediate and healed foci. The presence of Aschoff bodies indicates that this is a rheumatic myocarditis. Note also marked endocardial thickening due to inflammation and scarring, especially in the left atrium (MacCallum's patch).
|
Gross image questions
In the first image:
- Describe the gross findings of heart in the pericardial sac.
- Which process is occurring on the surface of the heart?
- Which heart sound would be associated with these gross findings?
In the second image:
- Describe the pathologic findings, particularly the appearance of the valves and the atrial wall.
VM image questions:
- Take a screen shot and annotate the:
- left ventricle, left atrium, the epicardial surface and the endocardial surface.
- Describe the epicardium and left atrial endocardium and relate the findings to the gross appearance of the heart.
- Take a screenshot and annotate:
- an Aschoff nodule/body and an Anitschkow cell (don’t spend more than 5 minutes looking).
Differential diagnosis questions:
25-1a. What is the differential diagnosis based on the initial clinical presentation?
25-1b. Taking the clinical findings and gross and microscopic features, what is the final diagnosis?
--ANSWER--
25-2. The microscopic images show macrophages with abundant cytoplasm and central round to oval nuclei with a central ribbon of chromatin that has been liked to “owl eyes” or “caterpillars”. Which of the following is the term for the pathognomonic cells in this disease?
- Anitschkow cells
- Aschoff bodies
- Lacunar cells
- Langerhans cells
- Reed-Sternberg cells
--ANSWER--
25-3. Which of the following is the proposed pathogenesis of this disease?
- Antibodies to streptococcus cross-react with heart antigens
- Bioactive products released by the tumor cause fibrosis
- Direct toxicity of catecholamines on cardiac myocytes
- Endocardial trauma acts as a nidus for sterile vegetations
- Mutations in sarcomeric proteins
--ANSWER--
25-4. Which of the following is the most common cause of mitral stenosis?
- Amyloidosis
- Carcinoid heart disease
- Nonbacterial thrombotic endocarditis
- Rheumatic heart disease
- Systemic lupus erythematosus
--ANSWER--
CASE NUMBER 512
(no virtual slides for this case)
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 19-year-old man is brought to the emergency department by ambulance following a syncopal episode that occurred while he was playing in a varsity basketball game 30 minutes earlier. Physical examination reveals a harsh systolic ejection murmur, ECG demonstrates prominent Q waves and echocardiography reveals left ventricular hypertrophy and asymmetric septal hypertrophy. Due to the severity of his disease, the patient was placed on a waiting list and eventually received a heart transplant. Gross and microscopic images of the explanted heart are provided.
Image Gallery:
|
Review Heart Histology
Slide 98HE
[DigitalScope]
Normal heart tissue sections demonstrate no evidence of fibrosis or hemorrhage. Cardiac myocytes have moderately sized centrally located nuclei. Normal myocytes are not brightly eosinphilic. Normally no inflammation is seen. Normal cardiac myocytes do not show hypertrophy.
Locate the atrioventricular sulcus that contains a branch of the coronary arterial system (a muscular artery that exhibits moderate intimal thickening) embedded in the epicardial fat. Look at the connective tissue present between the ventricle and atrium. This is part of the cardiac skeleton into which cardiac muscle inserts. A leaflet of an A-V valve takes origin from the cardiac skeleton. Look at the atrial and ventricular endocardium, consisting of an endothelial lining and the underlying connective tissue (the endothelium is often stripped away during processing, but there are some areas where it has been preserved). With low power, locate the Purkinje fibers present immediately beneath the ventricular endocardium (note the appearance of these fibers in cross and longitudinal orientations). These conducting fibers are larger and paler staining than the cardiac muscle fibers. Note the meshwork arrangement of the cardiac muscle fibers in the myocardium
|
Gross Findings
There is asymmetric septal hypertrophy resulting in bulging of the septal wall into the left ventricular outflow tract, giving rise to a banana-shaped ventricular lumen.
|
Microscopic Findings
There is myocyte hypertrophy and haphazard myocyte and myofibier disarray with interstitial fibrosis.
|
Differential diagnosis questions:
512-1a. What is the differential diagnosis based on the clinical findings?
512-1b. How does the echocardiography refine your diagnosis?
512-1c. What is the final diagnosis based on the gross and microscopic findings?
--ANSWER--
512-2. Analysis of a cardiac biopsy would most likely show which of the following?
- Abundant eosinophils
- Apple-green birefringent material
- Deletion of 1p
- Missense mutation in the b-myosin heavy chain gene
- Non-caseating granulomas
--ANSWER--
512-3. Which of the following is true regarding this disease?
- Etiology includes genetic and non-genetic causes.
- In women, it is most common in late pregnancy.
- Mutations in cytoskeletal proteins are seen in about 25% of cases.
- Patients receiving doxorubicin are at increased risk.
- The ejection murmur is due to ventricular outflow obstruction.
--ANSWER--
512-4. Which of the following gross findings is commonly seen at autopsy in these patients?
- “Banana-like” configuration of the left ventricular cavity
- Bilateral atrial dilation
- Commisural fusion
- Firm, plaque-like endocardial fibrous thickenings
- Mitral annular calcification
--ANSWER--
CARDIOVASCULAR PATHOLOGY Review Items
Key Vocabulary Terms (click here to search any additional terms on Stedman's Online Medical Dictionary)
CARDIOVASCULAR SYSTEM PATHOLOGY LEARNING OBJECTIVES
Goal 1: Heart Failure
Apply knowledge of anatomy, physiology, and general pathophysiologic principles to describe the clinical presentation associated with heart failure.
Objective 1: Right- and Left-Sided Heart Failure
Compare and contrast right heart versus left heart failure in terms of clinical features, pathologic features, and the short-term and long-term consequences.
Objective 2: Cardiomyopathy
Compare and contrast the clinicopathologic features of dilated, restrictive, and hypertrophic cardiomyopathies.
Goal 2: Cardiovascular Malformation
Apply knowledge of embryologic principles to describe how improper development of the heart and blood vessels leads to cardiac dysfunction.
Objective 1: Congenital Heart Disease
Name the most common forms of congenital heart disease and outline their clinical presentation, natural history, and long- and short-term complications.
Objective 2: Paradoxical Embolism
Describe a paradoxical embolus in terms of congenital heart disease and clinical presentation.
Objective 3: Cardiac Shunts
Compare and contrast left to right shunt and right to left shunt, and correlate with clinical presentation and short- and long-term consequences.
Goal 4: Cardiac Infection
Apply knowledge of immunological and microbiological principles to explain the role of infectious agents in myocardial dysfunction and describe the related clinical presentations.
Objective 1: Rheumatic Fever
Describe the major manifestations of rheumatic fever and its effect on the endocardium, myocardium, pericardium and valves.
Objective 2: Infective Endocarditis
Describe the major patterns of infective endocarditis and the pathologic changes seen in the cardiac valves.
Objective 3: Noninfective Endocarditis
Discuss the pathologic features of noninfective endocarditis on the cardiac valves.
Objective 4: Myocarditis
Describe the clinicopathologic features of myocarditis.
Objective 5: Pericarditis
Summarize the common causes of pericarditis and their pathophysiologic features.
Learning Goal 5: Valvular Dysfunction
Apply knowledge of the anatomy and physiology of heart valves to explain how valvular dysfunction leads to heart failure and describe the related clinical presentation.
Objective 1: Valve Stenosis
Discuss the complications associated with aortic stenosis.
Objective 2: Valve Insufficiency
Describe the clinicopathologic features of mitral valve prolapse.
Goal 6: Hypertension and the Heart
Apply knowledge of the mechanism of response of cardiac muscle to increased resistance to describe the clinical and pathologic changes seen in systemic and pulmonary hypertension.
Objective 1: Cardiac Changes in Pulmonary Hypertension
Describe the gross and microscopic adaptive changes in the myocardium that result from pulmonary hypertension.
Objective 2: Cardiac Changes in Systemic Hypertension
Discuss the pathogenesis of hypertension and the gross and microscopic adaptive changes in the myocardium that result from systemic hypertension.
|