|
|
Cell and Epithelial Tissue Structure Slide list:
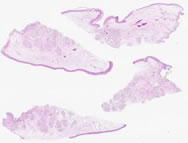
Slide Descriptions Specimen No. 2. Lung, human, H&E - Simple squamous (mesothelium, endothelium, epithelium) & pseudostratified columnar At low power, notice the general lack of cellularity indicative of the lung. Under higher magnification, pseudostratified columnar epithelium is seen in the bronchi and bronchioles, and cartilage can be seen surrounding many bronchi. The pseudostratified epithelium contains predominately ciliated columnar cells. Note the darker (eosinophilic)-staining band underlying the cilia. Each individual cilium is attached to the cell by a basal body. These basal bodies take up stain and, seen in aggregate, appear as a continuous band on light microscopy. Goblet cells and reserve (basal) cells can also be readily identified in the pseudostratified epithelial layer. Bronchi differ from the trachea in that they have a layer of smooth muscle between the mucosa and the submucosa. Note the mucous glands underlying the bronchial mucosa. Bronchioles are distinguished from bronchi by their lack of cartilage and submucosal glands. The epithelium of bronchioles also tends to be more cuboidal rather than columnar. In this section, congestion (filling of blood vessels with red blood cells) is present in blood vessels as well as in several alveolar spaces (which is not strictly a normal condition). This congestion highlights the alveolar capillaries and emphasizes the thin, delicate nature of the alveolar walls which facilitates gas exchange. Compare this to Slide 23, which is not congested. A lymphoid aggregate is present in association with bronchial mucosa (this is the so-called BALT, bronchial-associated lymphoid tissue). The delicate connective tissue of the pleura (the covering of the lung) is visible at the edge of the section, although only rare simple squamous mesothelial cells are evident.
Specimen No. 6. Kidney/adrenal, human, H&E - simple cuboidal, simple squamous, transitional (kidney) The large rectangular piece of tissue is the kidney. Clearly differentiated in this slide is the cortex and medulla of the kidney. The cortex is subdivided into two regions, the cortical labyrinth containing glomeruli (renal corpuscles) and the medullary rays comprised of the straight tubules of the ascending and descending limbs of Henle's loop as well as the collecting tubules. The medulla is composed of the collecting tubules (pale, cuboidal epithelium), and the vasa recta (capillaries that help to maintain osmotic gradients) forming a pyramidal structure. Find the renal pelvis. What type of epithelium lines the lumen? In the separate section of adrenal gland, one can clearly discern the cortex from the medulla. There are three zones in the cortex (zona glomerulosa, zona fasciculata, and zona reticularis); can you distinguish them? Note the superficial resemblance of the structures in the zona glomerulosa to the glomeruli in the kidney.
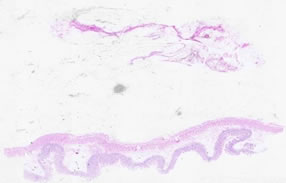
Specimen No. 15. Skeletal muscle/skin, human, H&E - stratified squamous (skin) Observe the characteristics of skeletal muscle (on the right): the presence of striations and the nuclei lined up on the outside of the fibers. View these two defining characteristics in both the longitudinal as well as the cross-sectioned orientations present on this slide. Striations are not typically visible on fibers in cross-section, but may be more easily seen in the longitudinal sections. The second sample on this slide (on the left) is skin. Notice the moderately thick layer of epidermis, including the (anuclear) stratum corneum. The dermis is the connective tissue layer underlying the epidermis and contains vasculature, eccrine sweat glands, hair follicles and their associated arrector pili (smooth) muscle. In this example, most of the hair follicles are cut in cross-section, which prevents following their length to the surface. Compare this epithelium with that shown in Slide 35.
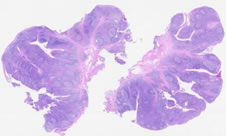
Specimen No. 34. Tonsil/salivary gland/skeletal muscle, human, H&E - stratified squamous (tonsil) The stratified squamous epithelium that covers the tonsil frequently dips into the underlying connective tissue, forming tonsillar crypts. The lymphoid cells within the tonsil can be seen either in aggregates or arranged as nodules containing germinal centers. A mucous-secreting salivary gland and a piece of skeletal muscle can also be seen in this section. Where is the muscle from?
Specimen No. 57. Adrenal, spleen, lymph node and thyroid, human, H&E - simple cuboidal (thyroid) Refer to the slide notes for slides 7, 9, 18, 22, and 32 for descriptions of adrenal, spleen and lymph node (copied below). Regarding the thyroid gland: The densely packed follicles that comprise the bulk of the thyroid are most notable for the homogeneous mass of colloid in the center. Note that both brown and white fat are present around the adrenal gland.
Specimen No. 27. Small bowel, human, H&E - simple columnar (small bowel) The villus structure of the mucosal surface indicates which organ this sample is from. Use your knowledge to determine the region of the small intestine. A small lymph node is present in the serosal fat.
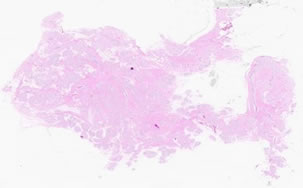
Specimen No. 8. Breast, human, H&E - stratified cuboidal (breast) This breast is composed of mainly fibrous connective tissue and a small amount of adipose tissue. Circular collections of glands (acini) are arranged into lobules. Note that the connective tissue between acini within a lobule is more thin and delicate than the dense connective tissue surrounding the lobules. The inactive glands on this slide are composed of two cell thick epithelium (cuboidal with underlying myoepithelium) in the small acini and ducts. The myoepithelium is found between the uppermost epithelial layer and the basal lamina and is the basis for the contractile nature of the duct. A two-layered epithelium may be more easily discerned in the larger ducts. The predominance of fibrous tissue and the small size of the lobular units are indicative of a small breast from a non-pregnant/non-lactating woman. Larger breasts contain more adipose tissue.
Specimen No. 35. Oral mucosa with salivary gland, human, H&E - stratified squamous and stratified cuboidal (oral mucosa with minor salivary glands) Compare the epithelium of this slide with the epithelium of the skin in Slide 15; what is the most striking difference between the two? The stroma underlying the non-keratinized stratified squamous epithelium in this slide is loose and highly vascularized. A gland containing predominantly mucous acini can also be found in this sample; based on this characteristic, which type of salivary gland is this?
Specimen No. 4. Colon, human, H&E - simple columnar epithelium (colon) The four layer structure of the GI tract is present in the colon just as in the small intestine and the stomach. However, villi are not present, nor are plicae circulares. Note the plasma cells and eosinophils present in the lamina propria. The muscularis mucosae that divides the mucosa from the submucosa is well-demonstrated in this section. The submucosa is comprised of a dense irregular connective tissue with vasculature. The longitudinal layer of the muscularis externa is condensed into prominent bands known as teniae coli. The straight, unbranched glands (crypts of Lieberkuhn) containing absorptive and goblet cells are indicative of the colonic origin of this slide. Compare this to Slide 25, which is also colon (but more variable in terms of how the glands are oriented).
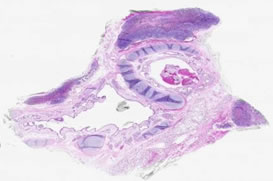
Specimen No. 14. Ureter, human, H&E - transitional (ureter) Notice that under low power, the entire wall of the ureter, as well as the lumen, are in the field of view (therefore this is a tube with a small diameter in vivo). The mucosa is composed of transitional epithelium that is characterized by the dome-shaped cells at the surface. These cells elongate when stretched, providing the ureter with its distensibility. The muscularis of the ureter has three layers: an inner longitudinal layer, a middle circular layer, and an outer longitudinal layer. The outermost layer of muscle can only be seen at the lower end of the ureter. Can you visualize it in this slide?
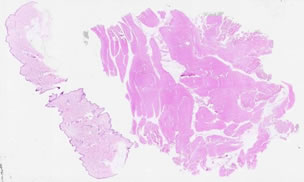
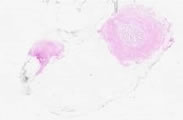
Specimen No. 10. Bronchi/lymph nodes, human, H&E - pseudostratified columnar (bronchi) The trachea divides into two branches, the bronchi which enter either the left or right lung. For this reason, many of the characteristics of this slide are similar to those found in samples of trachea, mainly the cellular components of the mucosa and the presence of the cartilage. The amount of cartilage present decreases down the length of each bronchus and the apparent elastic layer in the trachea is replaced by smooth muscle at the mucosal/submucosal boundary. The presence of blood and neutrophils in the lumen is not a normal condition. Several lymph nodes with classical germinal centers surround the bronchi. The heavy accumulation of (black) anthracotic pigment in thoracic lymph nodes is commonly seen in smokers and city dwellers. A small amount of poorly-aerated lung parenchyma is also present in this section.
Specimen No. 95. Urinary bladder, H&E - bladder (transitional) The transitional epithelium is located at the bottom of the section. The epithelial layer appears to be 2-5 cells thick, with no particular shape to the upper cells. The lack of the classic “dome shape” of the transitional epithelial cells combined with the relatively thin layers of smooth muscle layer indicate that this bladder was fixed when distended. The lamina propria that underlies the epithelium is composed of dense irregular connective tissue. There is no muscularis mucosae or submucosa. The smooth muscle (the muscularis propria) is arranged in 3 relatively indistinct bundles, oriented at right angles to each other. This is best seen toward the middle of the section, since the uppermost layer (relative to the epithelium that is at the bottom of the section) appears to be cut tangentially over much of the section. Note the different appearance of smooth muscle cut in cross-section vs. longitudinal section. A serosa is present underlying the muscularis propria. The serosa consists of loose fibroadipose tissue that is bounded by a layer of mesothelium arranged in a simple squamous arrangement. The presence of a serosal surface indicates that this section was taken from the superior surface of the bladder that forms part of the base of the peritoneal cavity.
|
||