|
|
Gastrointestinal tract Slide list:
Slide Descriptions Specimen No. 3. Stomach, human, H&E The stomach in this slide is well oriented at one end, but not at the other (similar to Slide 28 below). Focusing your attention at the good end (to the left), study the four layers that comprise the stomach. The mucosa consists of simple columnar surface epithelium and the underlying lamina propria that contains the gastric glands. The surface epithelial cells are mucin-secreting. Their cytoplasm is pale due to the mucin present above their nuclei. The muscularis mucosa is relatively thin and separates the mucosa from the submucosa that contains dense connective and adipose tissue and blood vessels. Thick layers of smooth muscle make up the muscularis externa. The serosa is the outermost layer. In the cardiac region, gastric glands are exclusively mucus-secreting and are loosely packed together with abundant intervening lamina propria. Glands in the fundus are relatively straight rather than coiled. The basal portion of the glands consists mainly of chief (pepsin-secreting) cells. Chief cells have a basally situated nucleus and typically stain gray-blue with hematoxylin and eosin. The central (isthmus) portions of the fundic glands contain primarily parietal cells (acid-secreting). Parietal cells are roughly triangular with a central nucleus, and their cytoplasm stains deep pink with H&E. The neck (uppermost region) of the fundic glands contains mixtures of chief, parietal, and mucous neck cells. The glands in the antrum resemble those of the cardiac region, however parietal cells are often found singly or in small groups in antral glands. Based on these distinctions, do you suspect that this longitudinal section is taken from the cardiac, fundic, or pyloric region? Identify the specialized types of epithelial cells indicative of this region. Note the folded nature (rugae) of the mucosa and submucosa. Based on the relationship of these folds to the muscularis mucosae, do you think these are permanent folds?
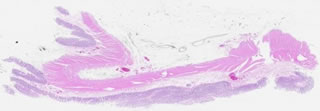
Specimen No. 4. Colon, human, H&E The four layer structure of the GI tract is present in the colon just as in the small intestine and the stomach. However, villi are not present, nor are plicae circulares. Note the plasma cells and eosinophils present in the lamina propria. The muscularis mucosae that divides the mucosa from the submucosa is well-demonstrated in this section. The submucosa is comprised of a dense irregular connective tissue with vasculature. The longitudinal layer of the muscularis externa is condensed into prominent bands known as teniae coli. The straight, unbranched glands (crypts of Lieberkuhn) containing absorptive and goblet cells are indicative of the colonic origin of this slide. Compare this to Slide 25, which is also colon (but more variable in terms of how the glands are oriented).
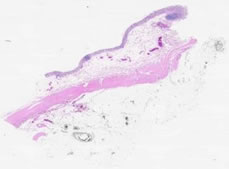
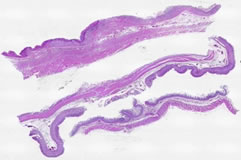
Specimen No. 12. Duodenum, human, H&E This slide shows 2 sections of 3 separate endoscopically-obtained biopsies from the duodenum. The biopsies contain the mucosa, muscularis mucosae, and small portions of the submucosa. The finger-like or leaf-like projections of mucosa are referred to as villi. The goblet cells and enterocytes that form the surface are easily distinguishable at higher magnification. Submucosal Brunner’s glands (branched tubular glands composed of columnar epithelium) are evident in one of the three pieces of tissue on this slide.
Specimen No. 13. Colon, human, H&E The epithelial surface is very fragmented and there is marking dye (black color specks) in the lamina propria in this example of large intestine. The submucosal and serosal layers are very prominent in this slide, however the serosa can only be viewed at low magnification. In areas where the epithelium is present, one can observe the lack of villi. The crypts of Lieberkuhn are now the predominant feature, extending from the surface to the muscularis mucosae.
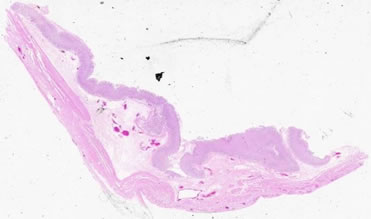
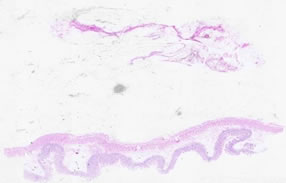
Specimen No. 16. Gall bladder, human, H&E The mucosa of the gall bladder consists of a tall simple columnar epithelium; this is the only cell type lining the gall bladder and thus helps distinguish this organ from others in the alimentary canal. Furthermore, the nuclei are located in the basal portion and microvilli, seen as a striated border, are at the apical portion of the epithelium. Lymphocytes can frequently be found around the lamina propria. The muscularis mucosae is absent. The muscularis underlying the mucosa is comprised of interlacing bundles of smooth muscle which, when contracted, results in the folding pattern of the mucosa that is commonly seen in histologic samples. Below the muscularis is the adventitia containing dense, irregular connective tissue, blood vessels, and adipose tissue. Diverticula of the mucosa, called Rokitansky-Aschoff sinuses, extend through the muscularis externa
Specimen No. 17. Small bowel, human, H&E In this slide, some areas are well-oriented to observe the villous structure of the mucosal surface, while other areas are cut in cross-section. Based on your knowledge of the defining characteristics of different regions of the small bowel, which region is demonstrated here? What evidence led you to that hypothesis?
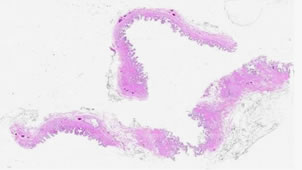
Specimen No. 24. Appendix, human, H&E This slide contains one longitudinal section and three cross sections of appendix. The presence of straight tubular glands extending to the muscularis mucosa and the organization of the muscularis externa (thick, inner circular layer surrounded by a thin longitudinal layer) may cause some confusion with other parts of the GI tract. However, the presence of extensive diffuse lymphatic tissue with some germinal centers in the lamina propria, as well as the small diameter seen in cross-section, help indicate which organ this truly is.
Specimen No. 25. Colon, human, H&E Refer to Slide 4 (notes copied below) for points of reference on colon and note that in this slide the orientation varies (i.e. glands are cut both longitudinally and in cross-section). The myenteric plexus is clearly visible between the layers of the muscularis externa in this section.
Specimen No. 26. Duodenum, human, H&E This section shows all 4 layers of the duodenum: mucosa, submucosa, muscularis externa, and serosa. Note the submucosal Brunner’s glands, which are characteristic of duodenum. The mucosa is less well-preserved in this section, but focally the villous structure can be clearly seen.
Specimen No. 27. Small bowel, human, H&E The villus structure of the mucosal surface indicates which organ this sample is from. Use your knowledge to determine the region of the small intestine. A small lymph node is present in the serosal fat.
Specimen No. 28. Stomach, human, H&E This slide, like Slide 3, is not well-oriented throughout the entire length. However, use the notes from Slide 3 to note the characteristics of stomach (copied below). Focus in on the different types of cells comprising the different types of glands in the mucosa.
Specimen No. 65. Gastroesophageal junction/fundus/jejunum, human, H&E Find the section with the gastroesophageal junction. Note the non-keratinized stratified squamous epithelium, and the glands in the lamina propria of the esophagus. These glands are called the esophageal cardiac glands, so named because of their similarity to the cardiac glands of the stomach. They are located in the terminal portion of the esophagus, and frequently also in the upper portion of the esophagus. Note the thick muscularis mucosae, which fades to become the much thinner muscularis mucosae of the stomach. The connective tissue of the submucosa is much thicker in the esophagus than in the stomach. Similarly, the muscularis externa of the esophagus is much thicker than the muscularis externa of the stomach. The gastric epithelium is much better preserved in the section from the gastric fundus. All four layers can be readily visualized in the section of jejunum. Note that only a moderate number of lymphocytes are present in the lamina propria. Villi are still present, with approximately equal numbers of absorptive and secretory (goblet) cells.
Specimen No. 73. Distal duodenum, human, H&E Some submucosal Brunner’s glands are present, allowing identification of this segment of small bowel as duodenum. Plicae circulares and villi are prominent. Note the central lymphatics of the villi. Can you see the striated border due to microvilli? The mucosa contains few goblet cells. Goblet cells increase in number as you move distally through the gut.
Specimen No. 84. Ileum, human, H&E This is a full thickness longitudinal section of the ileum, the terminal portion of the small bowel. The major feature that distinguishes the ileum from the jejunum is the abundance of single and aggregated lymphoid nodules. Large aggregates of lymphoid nodules in the ileum are called “Peyer’s patches”. Most of the lymphoid nodules in this section have germinal centers, indicating on-going immune reactions. Some of the germinal centers exhibit a “starry sky” pattern. Tingible body macrophages ingest apoptotic cells surrounding them, leaving a clear space that resembles a “star” in the “sky” of basophilic lymphocytes. The epithelium overlying Peyer’s patches is specialized for obtaining antigens (so-called M cells). It thus lacks the abundance of goblet cells that is seen in other portions of the epithelium. Note that permanent mucosal folds are present in this section (plicae circulares), as well as villi. The absorptive striated border on the intestinal epithelial cells, due to microvilli, is evident as a darker pink border on their apical surface. Paneth cells, with large acidophilic (red) granules at their apex are present at the base of many of the villi. Eosinophils (bi-nucleate with red granules) and plasma cells (clock-face chromatin and eccentric nuclear placement) are among the cell types recognizable in the lamina propria. You can confirm the longitudinal orientation of this section by noting that the inner layer of the muscularis externa is cut in cross-section, while the outer layer is cut longitudinally. Remember that in the small intestine, the inner layer of muscle is oriented circularly while the outer layer is longitudinal. Neurons and nerves of the myenteric plexus are located between the layers of the muscularis externa. The serosa is well-represented in this section and contains fat, blood vessels, and nerves. Most sections do not show the mesothelial-lined surface of the serosa, however.
|
||