|
|
Comprehensive Slide Guide
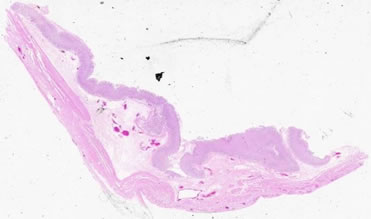
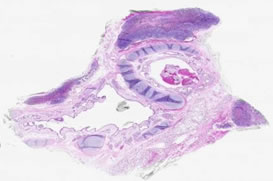
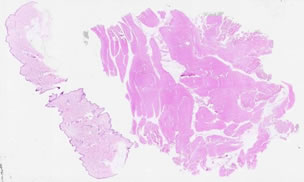
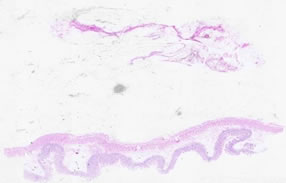
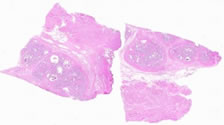
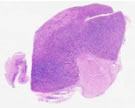
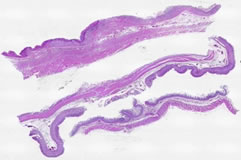
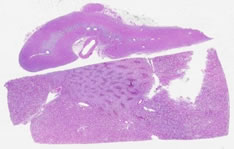
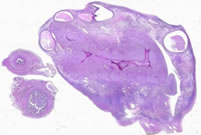
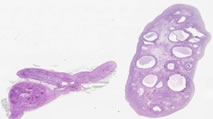
Specimen Descriptions Specimen No. 1. Ovary/fallopian tube, human, H&E The surface of the ovary is covered by a single layer of cuboidal epithelium, called the germinal epithelium. Follow the periphery of the ovarian tissue around the section. Small foci of germinal epithelium are visible, however, most of the germinal epithelium is not evident in this section. The germinal epithelium is continuous with the mesothelium that covers the mesovarium (the attachment of the ovary to the mesentery). The dense irregular connective tissue located between the germinal epithelium and the underlying cortex is called the tunica albuginea. Unlike the tunica albuginea of the testis, the ovarian tunica albuginea is not a distinct layer. The ovarian stroma is highly cellular, with a predominately spindle cell morphology. The ovarian medulla is located in the central portion of the ovary (this section is cut somewhat asymmetrically) and consists of loose connective tissue, convoluted blood vessels, lymphatics, and nerves. The endothelium on many of these vessels is well preserved and the smooth muscle layers on many arteries are easy to distinguish. The elastic laminae are not as readily apparent in these vessels, however. Clusters of follicles are seen superficially in the cortex of this section of ovary. Note the small primordial follicles containing a pale oocyte with a prominent nucleolus, surrounded by a single layer of squamous to cuboidal follicular cells. Some sections also contain a primary follicle with several layers of surrounding follicular cells and a prominent thick eosinophilic layer (the zona pellucida) surrounding the oocyte. Multiple secondary follicles are present, many surrounded by hemorrhage. This is a normal occurrence after ovulation; however, the presence of multiple hemorrhagic regions indicates some abnormality. Theca interna and externa cells can be seen at the periphery of some of the secondary follicles. An old corpus luteum (also called a corpora albicans) can also be found. This region is weakly eosinophilic and has a fluffy shape (which will become scarred down with time). A single cross-section of fallopian tube is also located on this slide. Note the ciliated simple columnar epithelium with a complex folding pattern.
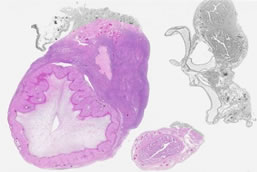
Specimen No. 2. Lung, human, H&E At low power, notice the general lack of cellularity indicative of the lung. Under higher magnification, pseudostratified columnar epithelium is seen in the bronchi and bronchioles, and cartilage can be seen surrounding many bronchi. The pseudostratified epithelium contains predominately ciliated columnar cells. Note the darker (eosinophilic)-staining band underlying the cilia. Each individual cilium is attached to the cell by a basal body. These basal bodies take up stain and, seen in aggregate, appear as a continuous band on light microscopy. Goblet cells and reserve (basal) cells can also be readily identified in the pseudostratified epithelial layer. Bronchi differ from the trachea in that they have a layer of smooth muscle between the mucosa and the submucosa. Note the mucous glands underlying the bronchial mucosa. Bronchioles are distinguished from bronchi by their lack of cartilage and submucosal glands. The epithelium of bronchioles also tends to be more cuboidal rather than columnar. In this section, congestion (filling of blood vessels with red blood cells) is present in blood vessels as well as in several alveolar spaces (which is not strictly a normal condition). This congestion highlights the alveolar capillaries and emphasizes the thin, delicate nature of the alveolar walls which facilitates gas exchange. Compare this to Slide 23, which is not congested. A lymphoid aggregate is present in association with bronchial mucosa (this is the so-called BALT, bronchial-associated lymphoid tissue). The delicate connective tissue of the pleura (the covering of the lung) is visible at the edge of the section, although only rare simple squamous mesothelial cells are evident.
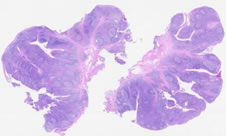
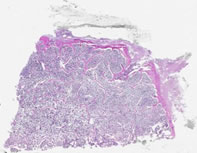
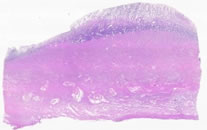
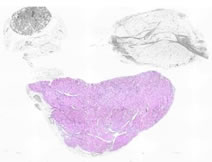
Specimen No. 3. Stomach, human, H&E The stomach in this slide is well oriented at one end, but not at the other (similar to Slide 28 below). Focusing your attention at the good end (to the left), study the four layers that comprise the stomach. The mucosa consists of simple columnar surface epithelium and the underlying lamina propria that contains the gastric glands. The surface epithelial cells are mucin-secreting. Their cytoplasm is pale due to the mucin present above their nuclei. The muscularis mucosa is relatively thin and separates the mucosa from the submucosa that contains dense connective and adipose tissue and blood vessels. Thick layers of smooth muscle make up the muscularis externa. The serosa is the outermost layer. In the cardiac region, gastric glands are exclusively mucus-secreting and are loosely packed together with abundant intervening lamina propria. Glands in the fundus are relatively straight rather than coiled. The basal portion of the glands consists mainly of chief (pepsin-secreting) cells. Chief cells have a basally situated nucleus and typically stain gray-blue with hematoxylin and eosin. The central (isthmus) portions of the fundic glands contain primarily parietal cells (acid-secreting). Parietal cells are roughly triangular with a central nucleus, and their cytoplasm stains deep pink with H&E. The neck (uppermost region) of the fundic glands contains mixtures of chief, parietal, and mucous neck cells. The glands in the antrum resemble those of the cardiac region, however parietal cells are often found singly or in small groups in antral glands. Based on these distinctions, do you suspect that this longitudinal section is taken from the cardiac, fundic, or pyloric region? Identify the specialized types of epithelial cells indicative of this region. Note the folded nature (rugae) of the mucosa and submucosa. Based on the relationship of these folds to the muscularis mucosae, do you think these are permanent folds?
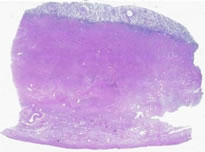
Specimen No. 4. Colon, human, H&E The four layer structure of the GI tract is present in the colon just as in the small intestine and the stomach. However, villi are not present, nor are plicae circulares. Note the plasma cells and eosinophils present in the lamina propria. The muscularis mucosae that divides the mucosa from the submucosa is well-demonstrated in this section. The submucosa is comprised of a dense irregular connective tissue with vasculature. The longitudinal layer of the muscularis externa is condensed into prominent bands known as teniae coli. The straight, unbranched glands (crypts of Lieberkuhn) containing absorptive and goblet cells are indicative of the colonic origin of this slide. Compare this to Slide 25, which is also colon (but more variable in terms of how the glands are oriented).
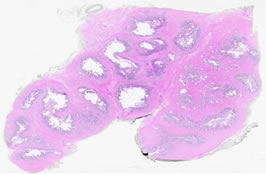
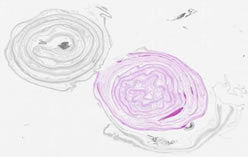
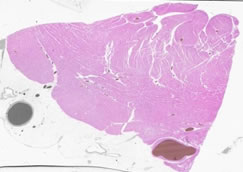
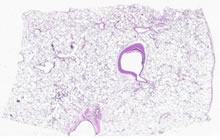
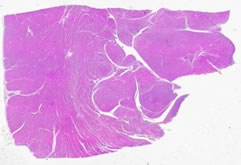
Specimen No. 5. Prostate/seminal vesicle, human, H&E The prostate is composed of bundles of smooth muscle, with sparse prostatic glands present in this section; note the two layer structure of the gland and the predominance of columnar to cuboidal epithelium lining the mucosal layer. Corpora amylacea, or prostatic concretions, are lamellated bodies found in the prostatic alveoli and are easily identifiable by their eosinophilic nature. The highly innervated nature of the prostate is visible due to the presence of several nerve ganglia in this section; observe under high power to visualize individual neurons. The neurons are large cells, with abundant pale eosinophilic cytoplasm and a prominent single nucleolus. Seminal vesicles are also seen in cross-section in this slide. The seminal vesicle mucosa can appear as "villi" due to the extensive folding. Examination using higher magnification reveals a loose connective tissue layer under the pseudostratified epithelium. Golden-brown lipofuschin pigment is prominent in the seminal vesicles, helping to distinguish this gland from the prostate. The prostatic urethra is also present in this section and is identifiable by the transitional epithelium.
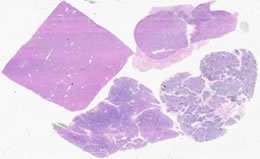
Specimen No. 6. Kidney (lower)/adrenal gland (upper), human, H&E The large rectangular piece of tissue is the kidney. Clearly differentiated in this slide is the cortex and medulla of the kidney. The cortex is subdivided into two regions, the cortical labyrinth containing glomeruli (renal corpuscles) and the medullary rays comprised of the straight tubules of the ascending and descending limbs of Henle's loop as well as the collecting tubules. The medulla is composed of the collecting tubules (pale, cuboidal epithelium), and the vasa recta (capillaries that help to maintain osmotic gradients) forming a pyramidal structure. Find the renal pelvis. What type of epithelium lines the lumen? In the separate section of adrenal gland, one can clearly discern the cortex from the medulla. There are three zones in the cortex (zona glomerulosa, zona fasciculata, and zona reticularis); can you distinguish them? Note the superficial resemblance of the structures in the zona glomerulosa to the glomeruli in the kidney.
Specimen No. 7. Adrenal gland/lymph node, human, H&E This adrenal gland (on the left) contains a prominent cortex. Note the three zones of the cortex. The zona glomerulosa is immediately superficial to the capsule. The nuclei appear crowded in this region due to the relative lack of cytoplasm in the parenchymal cells. These small cells are arranged in arching cords that are separated by elongated nuclei from the connective tissue stroma or the endothelial cells of capillaries. The next layer, zona fasciculata, contains cells with larger proportions of cytoplasm, but similar sized nuclei compared to glomerulosa cells. The cytoplasm has a spongy appearance due to the loss of lipid content in the preparation of this sample for H&E staining. The cells are oriented as radial cords, generally with a two cell width. The deepest layer, zona reticularis, is composed of relatively small cells oriented as interconnecting irregular cords. Capillaries and the occasional ganglion cell can be seen interspersed between the cords. A thin strip of more basophilic medulla can be seen in the central region of some portions of the gland. A lymphocyte-depleted lymph node with a large amount of anthracotic pigment (right) and a portion of lung with numerous pathologic conditions (center) can also be seen in this slide; use other slides to see a more normal histology for these organs. Compare this slide to Slide 57, which contains some adrenal tissue.
Specimen No. 8. Breast, human, H&E This breast is composed of mainly fibrous connective tissue and a small amount of adipose tissue. Circular collections of glands (acini) are arranged into lobules. Note that the connective tissue between acini within a lobule is more thin and delicate than the dense connective tissue surrounding the lobules. The inactive glands on this slide are composed of two cell thick epithelium (cuboidal with underlying myoepithelium) in the small acini and ducts. The myoepithelium is found between the uppermost epithelial layer and the basal lamina and is the basis for the contractile nature of the duct. A two-layered epithelium may be more easily discerned in the larger ducts. The predominance of fibrous tissue and the small size of the lobular units are indicative of a small breast from a non-pregnant/non-lactating woman. Larger breasts contain more adipose tissue. Compare this to Slide 59, showing lactational change.
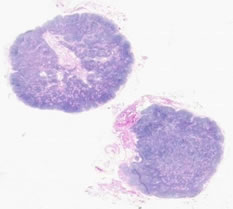
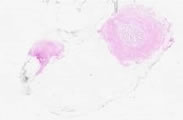
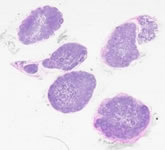
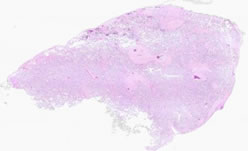
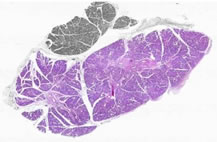
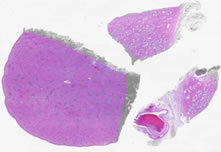
Specimen No. 9. Lymph nodes, human, H&E Two lymph nodes are present on this slide. Dense connective tissue forms the capsule that surrounds the lymph node. Trabeculae are contiguous portions of the capsule that penetrate into the cortex. The subcapsular sinus is immediately below the capsule and, can be seen as a space between the capsule and the lymph node parenchyma. This slide is NOT a wonderful example of classic germinal centers (see Slide 18 instead); however, the hilum with its blood vessels and lymphatics is quite obvious. Notice the dramatic differences between the architecture of the cortex and the medulla. The sinuses in these lymph nodes are filled with histiocytes which have pale eosiniphilic cytoplasm, making these regions stand out as pale regions in the lymph node medulla. See also Slide 22. Take a close look at blood vessels present within the lymph node. Many post-capillary venules with high (almost cuboidal) endothelium are present. These vessels are specialized to provided lymphocyte egress from the blood into the lymph node. For another comparison, refer to Slide 57, which contains some lymph node tissue.
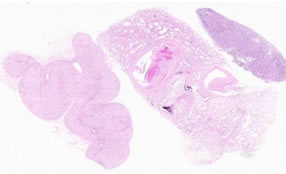
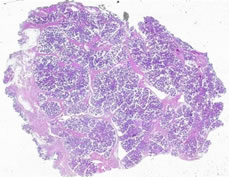
Specimen No. 10. Bronchi/lymph nodes, human, H&E - pseudostratified columnar (bronchi) The trachea divides into two branches, the bronchi which enter either the left or right lung. For this reason, many of the characteristics of this slide are similar to those found in samples of trachea, mainly the cellular components of the mucosa and the presence of the cartilage. The amount of cartilage present decreases down the length of each bronchus and the apparent elastic layer in the trachea is replaced by smooth muscle at the mucosal/submucosal boundary. The presence of blood and neutrophils in the lumen is not a normal condition. Several lymph nodes with classical germinal centers surround the bronchi. The heavy accumulation of (black) anthracotic pigment in thoracic lymph nodes is commonly seen in smokers and city dwellers. A small amount of poorly-aerated lung parenchyma is also present in this section.
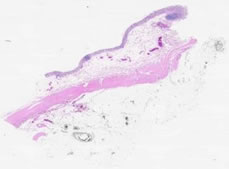
Specimen No. 11. Seminal vesicle, human, H&E Note the pseudostratifed columnar epithelium and the unique appearance of the secretory mucosa that results from the cross-sectioning of extensively folded sacs. The golden-brown lipofuschin pigment characteristic of the seminal vesicle is abundant. The mucosa covers a loose connective tissue layer (lamina propria) which overlays two layers of muscle, one circular and the other longitudinal. Find a nerve ganglion. The black color at the tissue periphery is marking dye that remains from the surgical sample. See also Slide 33.
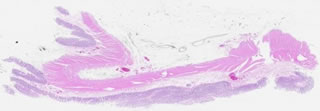
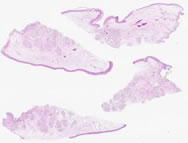
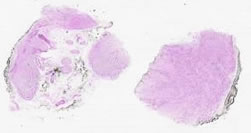
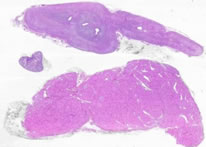
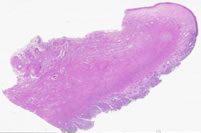
Specimen No. 12. Duodenum, human, H&E This slide shows 2 sections of 3 separate endoscopically-obtained biopsies from the duodenum. The biopsies contain the mucosa, muscularis mucosae, and small portions of the submucosa. The finger-like or leaf-like projections of mucosa are referred to as villi. The goblet cells and enterocytes that form the surface are easily distinguishable at higher magnification. Submucosal Brunner’s glands (branched tubular glands composed of columnar epithelium) are evident in one of the three pieces of tissue on this slide.
Specimen No. 13. Colon, human, H&E The epithelial surface is very fragmented and there is marking dye (black color specks) in the lamina propria in this example of large intestine. The submucosal and serosal layers are very prominent in this slide, however the serosa can only be viewed at low magnification. In areas where the epithelium is present, one can observe the lack of villi. The crypts of Lieberkuhn are now the predominant feature, extending from the surface to the muscularis mucosae.
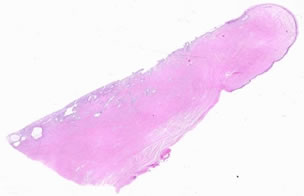
Specimen No. 14. Ureter, human, H&E Notice that under low power, the entire wall of the ureter, as well as the lumen, are in the field of view (therefore this is a tube with a small diameter in vivo). The mucosa is composed of transitional epithelium that is characterized by the dome-shaped cells at the surface. These cells elongate when stretched, providing the ureter with its distensibility. The muscularis of the ureter has three layers: an inner longitudinal layer, a middle circular layer, and an outer longitudinal layer. The outermost layer of muscle can only be seen at the lower end of the ureter. Can you visualize it in this slide?
Specimen No. 15. Skeletal muscle/skin, human, H&E Observe the characteristics of skeletal muscle (on the right): the presence of striations and the nuclei lined up on the outside of the fibers. View these two defining characteristics in both the longitudinal as well as the cross-sectioned orientations present on this slide. Striations are not typically visible on fibers in cross-section, but may be more easily seen in the longitudinal sections. The second sample on this slide (on the left) is skin. Notice the moderately thick layer of epidermis, including the (anuclear) stratum corneum. The dermis is the connective tissue layer underlying the epidermis and contains vasculature, eccrine sweat glands, hair follicles and their associated arrector pili (smooth) muscle. In this example, most of the hair follicles are cut in cross-section, which prevents following their length to the surface. Compare this to Slide 35 below.
Specimen No. 16. Gall bladder, human, H&E The mucosa of the gall bladder consists of a tall simple columnar epithelium; this is the only cell type lining the gall bladder and thus helps distinguish this organ from others in the alimentary canal. Furthermore, the nuclei are located in the basal portion and microvilli, seen as a striated border, are at the apical portion of the epithelium. Lymphocytes can frequently be found around the lamina propria. The muscularis mucosae is absent. The muscularis underlying the mucosa is comprised of interlacing bundles of smooth muscle which, when contracted, results in the folding pattern of the mucosa that is commonly seen in histologic samples. Below the muscularis is the adventitia containing dense, irregular connective tissue, blood vessels, and adipose tissue. Diverticula of the mucosa, called Rokitansky-Aschoff sinuses, extend through the muscularis externa
Specimen No. 17. Small bowel, human, H&E In this slide, some areas are well-oriented to observe the villous structure of the mucosal surface, while other areas are cut in cross-section. Based on your knowledge of the defining characteristics of different regions of the small bowel, which region is demonstrated here? What evidence led you to that hypothesis?
Specimen No. 18. Lymph node, human, H&E The major difference between this slide and Slide 9 is the presence of prominent germinal centers in these lymph nodes. See also Slide 22. For another comparison, refer to Slide 57, which contains some lymph node tissue.
Specimen No. 19. Uterus, human, H&E The majority of the tissue seen on this slide is myometrium, which is composed of bundles of smooth muscle. Spiral endometrial glands cut both longitudinally and in cross-section are evident at the surface, which has become detached from the rest of the uterine wall. Note the prominence of nerves and vessels amid the interlacing bundles of smooth muscle.
Specimen No. 20. Cervix, human, H&E Focus on the surface epithelium of the cervix. At the uterine end of the cervix (the endocervix), the epithelium is simple columnar, whereas a stratified squamous epithelium is present in the exocervix closer to the vagina. Note the squamo-columnar junction; the hemorrhage present is not normal, nor are the other areas of inflammation. Note the lack of keratinization of this stratified squamous epithelium, which helps to differentiate it it from the epidermis of skin. Cervical glands, which secrete a mucous substance to block entrance to the uterus or to facilitate the entry of sperm depending on the stage of the menstrual cycle and to lubricate the vagina, can be seen in this slide.
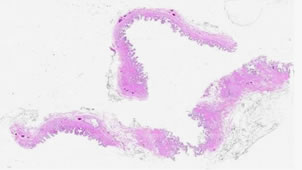
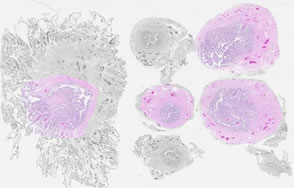
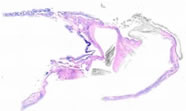
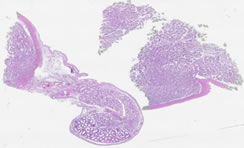
Specimen No. 21. Fallopian tube, human, H&E Six cross-sections of a fallopian tube can be observed in this slide, although all cannot be viewed at the higher magnifications. At low magnifications, the intricate folding of the mucosa (ciliated columnar epithelium) is noticeable in all sections. However, the extensiveness of the folds increases as the sample is taken from further away from the uterus. Deep to the mucosa is a thick layer of circular smooth muscle, a thin layer of longitudinal smooth muscle, as well as a highly cellular connective tissue and vasculature. Note that there is no debris in the lumen of the oviduct as there is in the seminal vesicles.
Specimen No. 22. Lymph node, human, H&E Refer to notes for Slide 9 and Slide 18 (excerpts copied below):
For another comparison, refer to Slide 57, which contains some lymph node tissue.
Specimen No. 23. Lung, human, H&E This sample of lung (as opposed to Slide 2) is well inflated and is not congested. An intrapulmonary lymph node with multiple germinal centers can be seen in this sample. Also note the presence of arteries and veins traveling together. Several bronchi, numerous little bronchioles and many alveoli can be found. Compare and contrast these different portions of the respiratory system.
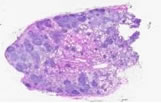
Specimen No. 24. Appendix, human, H&E This slide contains one longitudinal section and three cross sections of appendix. The presence of straight tubular glands extending to the muscularis mucosa and the organization of the muscularis externa (thick, inner circular layer surrounded by a thin longitudinal layer) may cause some confusion with other parts of the GI tract. However, the presence of extensive diffuse lymphatic tissue with some germinal centers in the lamina propria, as well as the small diameter seen in cross-section, help indicate which organ this truly is.
Specimen No. 25. Colon, human, H&E Refer to Slide 4 (notes copied below) for points of reference on colon and note that in this slide the orientation varies (i.e. glands are cut both longitudinally and in cross-section). The myenteric plexus is clearly visible between the layers of the muscularis externa in this section.
Specimen No. 26. Duodenum, human, H&E This section shows all 4 layers of the duodenum: mucosa, submucosa, muscularis externa, and serosa. Note the submucosal Brunner’s glands, which are characteristic of duodenum. The mucosa is less well-preserved in this section, but focally the villous structure can be clearly seen.
Specimen No. 27. Small bowel, human, H&E The villus structure of the mucosal surface indicates which organ this sample is from. Use your knowledge to determine the region of the small intestine. A small lymph node is present in the serosal fat.
Specimen No. 28. Stomach, human, H&E This slide, like Slide 3, is not well-oriented throughout the entire length. However, use the notes from Slide 3 to note the characteristics of stomach (copied below). Focus in on the different types of cells comprising the different types of glands in the mucosa.
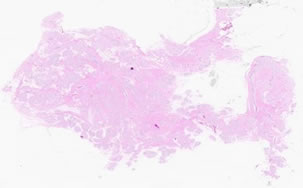
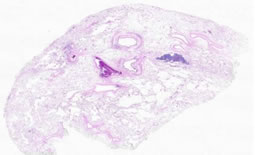
Specimen No. 29. Chorioamnionic membrane, human, H&E The membranes have been rolled and cut in cross-section to provide more area for evaluation. Examine the membrane roll on the right at higher magnification. Note the simple cuboidal epithelial lining of the amnion. The chorion is the more cellular, vacuolated layer deep to the amnion that carries the fetal vasculature.
Specimen No. 30. Placenta, human, H&E Note the chorionic villi, cut in cross-section, with their 2-layer covering of outer syncytiotrophoblast and inner layer of cytotrophoblast (the cytotrophoblast layer may only be evident focally). Clusters of syncytiotrophoblast cells called syncytial knots are also present. Branches of the umbilical arteries and veins are located within the chorionic villi. The deeply eosinophilic acellular material present on the surface of some villi is fibrin. Calcification, seen as bluish crystalline deposits, is present focally and is one indication of a mature placenta.
Specimen No. 31. Umbilical cord, human, H&E Note the vessels that are present: two arteries and one vein. The two arteries carry blood away from the fetal heart to the placenta and the vein is involved in returning blood to the fetus. The umbilical arteries lack an internal elastic lamina, and have a double layered muscular wall. An internal elastic lamina can be seen in the vein, which typically has a larger diameter than the two arteries. The muscle in the vein is thinner than in the artery, and consists of a single layer of circular smooth muscle. The connective tissue of the umbilical cord consists of Wharton's jelly which protects the umbilical vessels. Wharton's jelly is primarily hyaluronic acid and chondroitin sulfate, with delicate interlacing microfibrils and sparse collagen. The surface of the umbilical cord is a single layer of cuboidal to squamous amnionic epithelium.
Specimen No. 32. Spleen, human, H&E The dense capsule surrounding the spleen can be seen under low power; however, trabeculae are not readily apparent in this sample. Despite this downfall, the slide clearly illustrates the differences between white pulp (collections of lymphocytes) and red pulp where red blood cells are filtered. Furthermore, a thin ring of lymphocytes around central arteries can be seen in several fields of view; these are referred to as periarteriolar lymphatic sheaths. For another comparison, refer to Slide 57, which contains some tissue from the spleen.
Specimen No. 33. Seminal vesicle, human, H&E Refer to the notes for Slide 11 (copied below).
Specimen No. 34. Tonsil/salivary gland/skeletal muscle, human, H&E The stratified squamous epithelium that covers the tonsil frequently dips into the underlying connective tissue, forming tonsillar crypts. The lymphoid cells within the tonsil can be seen either in aggregates or arranged as nodules containing germinal centers. A mucous-secreting salivary gland and a piece of skeletal muscle can also be seen in this section. Where is the muscle from?
Specimen No. 35. Oral mucosa with salivary gland, human, H&E Compare the epithelium of this slide with the epithelium of the skin in Slide 15; what is the most striking difference between the two? The stroma underlying the non-keratinized stratified squamous epithelium in this slide is loose and highly vascularized. A gland containing predominantly mucous acini can also be found in this sample; based on this characteristic, which type of salivary gland is this?
Specimen No. 36. Heart, left ventricular free wall, human, H&E Cardiac muscle is the most pronounced feature of this slide with nuclei being found inside fibers and fibers interconnecting. Striations can be visualized in some areas where cells are cut longitudinally. Vessels can be seen in the wall of this heart as well; the lumens contain barium that was injected to determine vessel patency.
Specimen No. 37. Heart, left ventricular free wall, human, V.V. Masson This stain highlights the location of connective tissue within the heart (collagen stains green). The green dye can be seen around vessels and bundles of myocytes in this sample of cardiac muscle. Note that barium (used for post-mortem radiographic determination of vascular patency) is present in the lumen of many vessels.
Specimen No. 38. Aorta, human, H&E The lining of endothelial cells in the tunica intima can be seen in patches on this slide; however, the collagen fibers and elastic lamellae that comprise the remainder of the intima are apparent. The middle layer, tunica media, is composed of an abundance of smooth muscle and elastic material arranged as fenestrated membranes, rather than as fibers. The tunica adventitia, the outermost layer, is the location of the vasa vasorum (blood vessels) and the nervi vascularis (nerves) that supply the arterial wall and can be found around the collagenous fibers that form the bulk of the adventitia
Specimen No. 39. Aorta, human, V.V. Masson This staining allows us to visualize the different components of each layer of the aorta due to the fact that fibrous connective tissue stains green, elastic fibers black, and smooth muscle red. The intima can be best seen in tangential cut at one end of the section, with black-stained elastic fibers surrounded by green-stained connective tissue, rather than the combination of black-stained elastic fibers and red-stained smooth muscle seen in the media.
Specimen No. 40. Thymus, human, H&E Each lobule of the thymus contains a basophilic cortex and a less basophilic medulla. The cortex contains numerous densely packed lymphocytes. The medulla has fewer lymphocytes, which allows the visualization of epithelioreticular supporting cells and macrophages, which can be difficult to distinguish from each other. The medulla also possesses numerous eosinophilic and paucicellular structures called Hassall’s bodies (Hassall’s corpuscles) that are characteristic of the thymus. Hassall’s bodies are composed of terminally differentiated thymic epithelial cells. For another comparison, refer to Slide 58, which contains some tissue from the thymus.
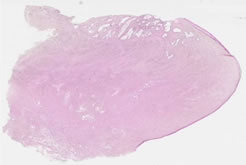
Specimen No. 41. Dorsal root ganglion, human, H&E LFB With this modified H&E/Luxol fast blue staining protocol, myelin stains blue and lipofuschin stains yellow. Note the elongated nuclei of the Schwann cells and the satellite cells that surround the neurons. The nucleoli are very apparent within the pale staining nuclei of the sensory neurons.
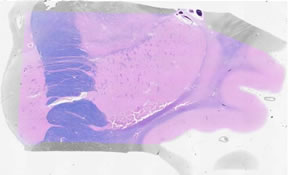
Specimen No. 42. Midbrain, human, H&E/LFB Features of this section include the 3d cranial nerve and the myelinated cerebral peduncle. Can you find the pigmented neurons of the substantia nigra? These neurons contain neuromelanin, which is a precursor of dopamine. The cerebral aqueduct on this section appears as a cystic space lined by ciliated cuboidal epithelium (the cilia are difficult to see in most sections). You can also see the myelinated fibers of the corticospinal tract, surrounded by the oligodendroglial cells that make the myelin.
Specimen No. 43. Thalamus, human, H&E/LFB The most important feature of this section is the pineal gland, which contains neurosecretory elements. The mineralization seen is common. In birds, the magnetite (iron) content of the pineal is thought to be important in directing migration. The back of the 3d ventricle, surrounded by the choroid plexus (cuboidal epithelium) is also seen in the lower right of this section.
Specimen No. 44. Cerebral cortex, human, H&E/LFB The arachnoid layer of delicate connective tissue can be visualized focally, along with its underlying pia mater, a single cell layer directly on the cortex. The cerebral gray matter appears pink in this stain. The neurons in the gray matter have a prominent single nucleolus, with basophilic areas of cytoplasm. This is the Nissl substance, which actually is RNA. The white matter appears blue due to its high myelin content. Astrocytes are large and round. Oligodendroglia have a lymphocyte-like appearance.
Specimen No. 45. Hippocampus, human, H&E/LFB A branch of the posterior cerebral artery is present in the center of the section. Note also the choroid plexus, consisting of ependymal cells and cuboidal cells. Capillaries are visible in the central parts of the loops. Mineralization of the choroid plexus is commonly observed. The choroid plexus makes the cerebrospinal fluid. Note the large pyramidal neurons of the hippocampus itself. Dentate neurons are arranged in rows. Note that the internal elastic lamina of arteries stains blue with this stain. The small ovoid /spindle cells are microglia; the perineuronal oligodendroglia have nuclei that resemble lymphocytes.
Specimen No. 46. Thalamus, human, H&E/LFB Note the ependymal surface on the medial edge. Six to 12 clusters of neurons (called nuclei) can be seen in this section. The internal capsule is visualized here by its high myelin (stains bright blue with LFB stain) content.
Specimen No. 47. Cingulate gyrus/ corpus callosum, human, H&E/LFB The meninges (arachnoid and pia) can be seen on one side of the tissue, with the ependyma on the other side. The cingulate gyrus has a similar histologic appearance to the cortex.
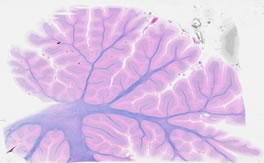
Specimen No. 48. Cerebellum, human, H&E/LFB Note the characteristic folia and gyrae of this tissue. The arachnoid envelopes the folia. The layers are: the relatively acellular molecular layer, the Purkinje cell layer, and the granular cell layer. This is a good place to identify microglia. Myelinated tracts and the ependyma of the 4th ventricle are present on this section.
Specimen No. 49. Medulla, human, H&E/LFB This section demonstrates the floor of the 4th ventricle, pyramidal tracts, the (irregularly shaped) inferior olivary nucleus. Cranial nerve nuclei are visible in the floor of the 4th ventricle.
Specimen No. 50. Basal ganglia, human, H&E/LFB The insula resembles cortex histologically. Myelinated tracts include the extreme capsule, the claustrum, and the external capsule. The putamen has a striated appearance. The globus pallidus appears somewhat speckled here. The internal capsule is the very large myelinated tract. The caudate nucleus is also present, with ependyma adjacent.
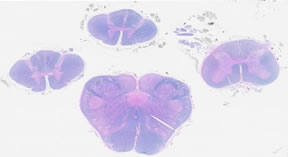
Specimen No. 51. Spinal cord, human, H&E/LFB The 4 sections on this slide are taken from the lower medulla, upper cervical, mid-cervical, and lumbar regions of the spinal cord. Note that both neurons and myelinated tracts are present in these sections. The neurons are present in the gray matter in the central portion of the cord, surrounded by the myelinated axons of the white matter. The roots of various spinal nerves are seen in this section, but not the dura.
Specimen No. 52. Cervix, human, H&E The cervix essentially bridges the uterus and the vagina, and thus changes in the histology of this tissue can be observed along its length. The mucosa of the external os (exocervix) contains stratified squamous epithelium that is similar to the vagina. The internal os (endocervix) has simple columnar epithelium that is similar to the lining of the uterus. Note that glands are only apparent underlying the endocervical mucosa. Furthermore, compare the tissue that underlies the epithelial surfaces in both regions. What differences do you observe?
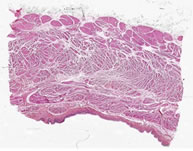
Specimen No. 53. Myenteric plexus, human, H&E A thin connective tissue layer is located between layers of the muscularis externa layer of the gastrointestinal tract. Occasional clusters of neurons can be found in this connective tissue. These are part of the myenteric plexus (Auerbach’s plexus). These neurons are important for coordinating the muscular movements that propel food through the digestive tract (peristalsis).
Specimen No. 54. Pituitary, human, H&E and LFB The pituitary gland is differentiated into two regions: the adenohypophysis (anterior) and the neurohypophysis (posterior). The adenohypophysis contains cells that are chromophobes (stain poorly) and chromophils (stain well with either basic or acidic dyes, the basophils and acidophils, respectively). The neurohypophysis is less cellular and contains nonmyelinated nerve fibers and pituicytes (which are comparable to neuroglial cells of the CNS). Some colloid areas stain a brilliant blue. For another comparison, refer to Slide 58, which contains some tissue from the thymus.
Specimen No. 55. Dural sinus, human, H&E The dural sinuses are simply veins that have an atypical structure due to their location. What is seen in this sample are spaces in the dura mater that are lined with endothelial cells in order to form a venous channel.
Specimen No. 56. Sympathetic ganglion, human, H&E The most pronounced feature of this slide is the sheer number of neurons that can be observed. What characteristics of this ganglion can you use to differentiate this from ovary? Disregard the marking pigment that can be seen in several fields of view.
Specimen No. 57. Adrenal, spleen, lymph node and thyroid, human, H&E Refer to the slide notes for slides 7, 9, 18, 22, and 32 for descriptions of adrenal, spleen and lymph node (copied below). The densely packed follicles that comprise the bulk of the thyroid are most notable for the homogeneous mass of colloid in the center. Note that both brown and white fat are present around the adrenal gland.
Specimen No. 58. Thymus, pituitary, pancreas, and liver, human, H&E The pancreas is basophilic at low power due to the high content of rough endoplasmic reticulum and Golgi that is necessary for protein production and secretion. The acini are well preserved in this section and the intralobular and interlobular ducts with their simple columnar epithelium are also prominent. The pale eosinophilic areas are the Islets of Langerhans. The thymus is also basophilic at low power due to the high concentration of nuclei (lymphocytes have very little cytoplasm). Lobules contain a cortex of densely arranged thymocytes in the outermost portions, with less densely populated (paler) medulla in the center. Hassall’s bodies are located within the medulla. See also slide notes for Slide 40.
Pituitary: See slide notes for Slide 54 for these sections. This particular piece of tissue shows mostly anterior pituitary.
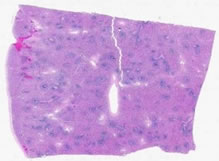
The square piece of liver is eosinophilic at low power due to the large amount of cytoplasm in the hepatocytes. Note the small, fat globules in some hepatocytes. Identify portal tracts and their component parts (hepatic artery, portal vein, and a bile duct). Note the ray-like pattern of the hepatocytes and the sinusoids that lead to the central vein.
Specimen No. 59. Breast with lactational change, human, H&E Compare this slide with that of normal breast seen in Slide 8. The acini in this slide are convoluted and markedly enlarged relative to non-lactating breast. Lobules likewise seem to contain more acini than in non-lactating breast. Note the eosinophilic secretions in the lumen. The background stroma in this tissue is predominantly collagenous fibrous tissue, rather than the adipose tissue which is more commonly seen in breast biopsies.
Specimen No. 60. Submandibular (salivary) gland, human, H&E The submandibular gland contains three types of acini: serous, mucous, and mixed (serous and mucous). Compare this distribution of glands to seen in the parotid gland in Slide 61 below. Can you identify serous demilunes in some of the mixed acini? The larger excretory ducts have pseudostratified columnar epithelium. The medium-sized striated ducts have simple columnar epithelium. They stand out due to their relative eosinophilia relative to the salivary acini. The acini are arranged into lobules separated by loose connective tissue. Larger vessels and ducts are present between the lobules. Note the fibrous capsule visible on one side of the section.
Specimen No. 61. Parotid (salivary) gland, human, H&E The parotid gland can be easily distinguished from the other salivary glands since it is composed only of serous acini. As in the submandibular gland (Slide 60), striated ducts are readily apparent due to their relative eosinophilia. The small intercalated ducts can also be seen in this section, as they are more eosinophilic than the serous acini themselves. The relative eosinophilia may vary due to staining conditions; note also the differences in cellular detail of the ducts relative to the acini. The parotid gland characteristically contains more adipose tissue than the submandibular and sublingual glands, as demonstrated here. Note that acini are divided into lobules by dense connective tissue. Larger ducts and vessels are located within the connective tissue separating the lobules. The facial nerve (cranial nerve VII) passes through the substance of the parotid gland. Can you find the facial nerve in this section?
Specimen No. 62. Parathyroid gland, human, H&E The parathyroid gland is covered by a thin fibrous capsule. The majority of the cells are chief cells, characterized histologically by small size, with a small amount of clear to pale eosinophilic cytoplasm. The nuclei of chief cells are strongly basophilic with condensed chromatin. Patches of oxyphil cells are also present. The nuclear features of oxyphil cells are similar to those of chief cells, however oxyphil cells have large amounts of strongly eosinophilic granular cytoplasm. This particular parathyroid gland also contains a large amount of adipose tissue. For another comparison, refer to Slide 64, which contains tissue from the parathyroid.
Specimen No. 63. Vas deferens, human, H&E This slide contains two complete cross-sections of vas deferens (a.k.a. ductus deferens). Note the small diameter of these cross-sections by holding the slide up to the light. The vas contains 3 layers: mucosa, muscularis, and adventitia. The mucosa contains pseudostratified columnar epithelium. Stereocilia are present at the mucosal surface, but are not well visualized on this slide. The muscularis is three layered, with inner and outer longitudinal and middle circular layers. The adventitia is composed of loose connective tissue.
Specimen No. 64. Parathyroid/thyroid/adrenal, human, H&E The features of the parathyroid gland are discussed for Slide 62. Oxyphil cells are rare in this section, which also contains minimal adipose tissue. This gland is sectioned across the hilum. Hilar structures (major vessels) are visible in the center of the section. The thyroid gland contains numerous follicles filled with homogeneously staining eosinophilic colloid. Note the simple cuboidal epithelium. All of the layers of cortex and medulla are easy to discern in this section of adrenal gland. The medulla is larger than in the previous examples of adrenal gland in this slide set. Note that several nerve ganglia and many nerves are present around the gland periphery.
Specimen No. 65. Gastroesophageal junction/fundus/jejunum, human, H&E Find the section with the gastroesophageal junction. Note the non-keratinized stratified squamous epithelium, and the glands in the lamina propria of the esophagus. These glands are called the esophageal cardiac glands, so named because of their similarity to the cardiac glands of the stomach. They are located in the terminal portion of the esophagus, and frequently also in the upper portion of the esophagus. Note the thick muscularis mucosae, which fades to become the much thinner muscularis mucosae of the stomach. The connective tissue of the submucosa is much thicker in the esophagus than in the stomach. Similarly, the muscularis externa of the esophagus is much thicker than the muscularis externa of the stomach. The gastric epithelium is much better preserved in the section from the gastric fundus. All four layers can be readily visualized in the section of jejunum. Note that only a moderate number of lymphocytes are present in the lamina propria. Villi are still present, with approximately equal numbers of absorptive and secretory (goblet) cells.
Specimen No. 66. Lungs/pleura, human, H&E Find the pleural surface. Simple squamous mesothelial cells line the pleural surface, with underlying dense connective tissue. Can you identify the collagen bundles? This lung was well-inflated prior to fixation, so it is easy to appreciate the thinness of the alveolar septae. A partial cross-section of a large bronchus is at one end of the section. Note the cilia on the pseudostratified columnar epithelium, submucosal mucous glands, and the cartilage. The cartilage is normally basophilic, however it appears somewhat eosinophilic on this section. Numerous plasma cells are present in the submucosa of the bronchus.
Specimen No. 67. Bone marrow, human, H&E A thin layer of compact/dense bone borders this section, with internal cancellous/spongy bone. The spaces between bony spicules are filled with hematopoietic cells. Not the large numbers of (round, empty) fat cells present within the marrow space. The fat is lost during processing into paraffin sections. Megakaryocytes can be readily identified, since they are approximately 5-fold larger than most bone marrow cells and contain strongly eosinophilic cytoplasm and multiple nuclei. Can you distinguish the myeloid cells from the erythroid cells in the marrow space?
Specimen No. 68. Prostate/nerve ganglia/spleen, human, H&E The largest piece of tissue on this slide is the spleen. The splenic capsule is composed of dense connective tissue, which dips into the parenchyma to form trabeculae. The white pulp appears blue by H&E due to the large numbers of lymphocytes with very little cytoplasm. Many of these lymphocytes can be seen surrounding the central arterioles (the periarteriolar lymphoid sheath). Central arteries are not always visible in the plane of the section. Note the types of cells present in the red pulp versus the white pulp. The prostate demonstrates somewhat complex glands due to folding. The fibromuscular stroma is well-preserved. Note that numerous nerves and nerve ganglia surround the prostate, which has no true capsule.
Specimen No. 69. Kidney/adrenal, human, H&E Both cortex and medulla are represented in the adrenal section. The kidney has both cortex, with glomeruli and tubules, and medulla. The medullary rays are present in both longitudinal and cross-section in the central portion of the kidney section. Note the thin fibrous capsule.
Specimen No. 70. Heart, human, H&E The epicardium is present on one side of this section. Note the distinguishing characteristics of the myocardium: the branching fibers, the central nuclei, and the striations (best seen in longitudinal section).
Specimen No. 71. Liver/pancreas, human, H&E The liver is the large square of tissue on this slide. A focal area has attached capsule - the majority of the capsule has become detached from the section. Note the anastomosing chords of hepatocytes, with intervening sinuses lined by Kupffer cells. Locate portal tracts containing bile ducts and portal veins. The central veins are somewhat less conspicuous. The pancreas tissue is rectangular. Some autolysis has occurred. The islets are not prominent by color, but can be distinguished on close inspection. Large pancreatic ducts lined by columnar epithelium are located centrally.
Specimen No. 72. Testis/epididymis, human, H&E At least two pieces of testis are present on this slide. Note the thick capsule, the tunica albuginea. The parenchyma of the testis is composed of seminiferous tubules. Rare sperm are present in the lumen in this 14 year old patient. The epididymis is cut in multiple cross-sections, which demonstrate the pseudostratified columnar epithelium. The long stereocilia are evident, with a prominent terminal bar. These structures are not true cilia and do not "beat". Abundant debris is present in the lumen.
Specimen No. 73. Distal duodenum, human, H&E Some submucosal Brunner’s glands are present, allowing identification of this segment of small bowel as duodenum. Plicae circulares and villi are prominent. Note the central lymphatics of the villi. Can you see the striated border due to microvilli? The mucosa contains few goblet cells. Goblet cells increase in number as you move distally through the gut.
Specimen No. 74. Peripheral blood smear, AML, human, Wright-Giemsa This specimen of peripheral blood is NOT normal. It was obtained from a patient with a hematologic malignancy (acute promyelocytic leukemia) that resulted in the circulation of immature cells that are normally present only in the bone marrow. The purpose of this slide is to give you some experience in distinguishing these immature white blood cells from the mature white blood cells usually seen in the blood.
Specimen No. 75. Peripheral blood smear, CLL, human, Wright-Giemsa Again, this blood smear is NOT normal. It is from a patient with a hematologic malignancy (lymphoma) that resulted in approximately 50% circulating eosinophils. Since eosinophils are usually rare in peripheral blood, examination of this slide provides you a chance to better learn to recognize these cells.
Specimen No. 76. Uterus/endometrium, human, H&E The endometrium on this well-oriented section of uterus shows tall columnar surface epithelium, with spiral glands extending down into the highly cellular endometrial stroma. The underlying myometrium consists predominately of bundles of smooth muscle, with prominent blood vessels and nerves. Note the presence of more connective tissue near the serosal surface.
Specimen No. 77. Ovary/fallopian tube, human, H&E The most prominent structure in this ovary is the corpus luteum. The corpus luteum is composed of oval to polygonal, highly eosinophilic cells with abundant cytoplasm and prominent nucleoli. The ovarian medulla containing many blood vessels is also prominent in this section. Two sections of fallopian tube are present. Note the vessels, nerves, and smooth muscle present in the wall of the fallopian tube. One of the tubes also shows a small paratubal fluid-filled cyst. Examine the epithelium using the high dry or oil objective to visualize the cilia present on the columnar epithelial cells.
Specimen No. 78. Cervix, human, H&E Follow the epithelial surface of this tissue around the entire section. Note the transition from the stratified squamous epithelium of the exocervix to the columnar epithelium of the endocervix at the squamo-columnar junction. The endocervix has abundant underlying glands that provide cervical mucus. Identify the smooth muscle present deeper in the section.
Specimen No. 79. Uterus/endometrium, human, H&E This section is cut tangentially, causing the endometrial thickness to appear much thicker at one end of the section. Some slides also show an artifactual lack of staining in the upper endometrium. This endometrium is secretory, day 20-22.
Specimen No. 80. Uterus/endometrium, human, H&E The secretory endometrial glands profiles are complex. Spiral arteries are prominent.
Specimen No. 81. Ovary/adrenal, human, H&E The ovary contains numerous follicles in various stages of maturation. Primordial follicles, consisting of an oocyte surrounded by a single layer of squamous epithelium, are numerous in the cortex. Some early primary follicles can also be seen. Most of the prominent follicles are the secondary follicles. Although the oocyte may not be present in all sections, one mature follicle with a well-developed cumulus oophorus can be identified.
Specimen No. 82. Peripheral blood smear, typical, human, Wright-Giemsa This slide demonstrates the typical appearance and cellularity of a peripheral blood smear.
Specimen No. 83. Ovary with corpus luteum/fallopian tube, human, H&E This is an excellent example of an ovary with a prominent corpus luteum occupying approximately 50% of the organ. Two sections of fallopian tube are also present on this slide. Can you identify the paratubal cysts? Although not strictly normal, these tubal cysts are prevalent and rarely cause problems for the patient.
Specimen No. 84. Ileum, human, H&E This is a full thickness longitudinal section of the ileum, the terminal portion of the small bowel. The major feature that distinguishes the ileum from the jejunum is the abundance of single and aggregated lymphoid nodules. Large aggregates of lymphoid nodules in the ileum are called “Peyer’s patches”. Most of the lymphoid nodules in this section have germinal centers, indicating on-going immune reactions. Some of the germinal centers exhibit a “starry sky” pattern. Tingible body macrophages ingest apoptotic cells surrounding them, leaving a clear space that resembles a “star” in the “sky” of basophilic lymphocytes. The epithelium overlying Peyer’s patches is specialized for obtaining antigens (so-called M cells). It thus lacks the abundance of goblet cells that is seen in other portions of the epithelium. Note that permanent mucosal folds are present in this section (plicae circulares), as well as villi. The absorptive striated border on the intestinal epithelial cells, due to microvilli, is evident as a darker pink border on their apical surface. Paneth cells, with large acidophilic (red) granules at their apex are present at the base of many of the villi. Eosinophils (bi-nucleate with red granules) and plasma cells (clock-face chromatin and eccentric nuclear placement) are among the cell types recognizable in the lamina propria. You can confirm the longitudinal orientation of this section by noting that the inner layer of the muscularis externa is cut in cross-section, while the outer layer is cut longitudinally. Remember that in the small intestine, the inner layer of muscle is oriented circularly while the outer layer is longitudinal. Neurons and nerves of the myenteric plexus are located between the layers of the muscularis externa. The serosa is well-represented in this section and contains fat, blood vessels, and nerves. Most sections do not show the mesothelial-lined surface of the serosa, however.
Specimen No. 85. Thyroid/adrenal/adipose tissue, human, H&E The largest piece of tissue on the slide is the thyroid. This tissue consists of follicles lined by simple cuboidal epithelium and filled with homogeneous eosinophilic colloid. The variations in size, shape, and preservation of follicles represent normal variations. The parathyroid gland contains chief and oxyphil cells, with a moderate amount of adipose tissue within the gland. The majority of the cells are chief cells. Oxyphil cells are rare and present only in small clusters. A nerve twig is evident in the adipose tissue outside the gland. The 3d piece of tissue on the slide is white adipose tissue from the anterior mediastinum. The adipocytes appear empty due to loss of the large lipid vacuole during tissue processing. When present, nuclei are flattened and pressed to the outside edge of the cell. Note the abundance of capillaries and small blood vessels. A few larger blood vessels are present. Some of these are associated with mild hemorrhage as a result of the tissue procurement process.
Slides 86 – 94 each contain samples of multiple types of mouse tissue. A guide to these slides will be provided during the unit on comparative histology.
Specimen No. 95. Urinary bladder, H&E - bladder (transitional) The transitional epithelium is located at the bottom of the section. The epithelial layer appears to be 2-5 cells thick, with no particular shape to the upper cells. The lack of the classic “dome shape” of the transitional epithelial cells combined with the relatively thin layers of smooth muscle layer indicate that this bladder was fixed when distended. The lamina propria that underlies the epithelium is composed of dense irregular connective tissue. There is no muscularis mucosae or submucosa. The smooth muscle (the muscularis propria) is arranged in 3 relatively indistinct bundles, oriented at right angles to each other. This is best seen toward the middle of the section, since the uppermost layer (relative to the epithelium that is at the bottom of the section) appears to be cut tangentially over much of the section. Note the different appearance of smooth muscle cut in cross-section vs. longitudinal section. A serosa is present underlying the muscularis propria. The serosa consists of loose fibroadipose tissue that is bounded by a layer of mesothelium arranged in a simple squamous arrangement. The presence of a serosal surface indicates that this section was taken from the superior surface of the bladder that forms part of the base of the peritoneal cavity. See also Slide 97 and Slide 98, which contain urinary bladder tissue.
Specimen No. 96. Muscle-tendon junction, H&E In this section, skeletal muscle is located to the left, merging into the tendon on the right. The skeletal muscle is cut longitudinally, allowing you to see the striations well in multiple areas of the section. Note the nuclei are present on the outside of the skeletal muscle fibers. The connective tissue on the outside of the mass of skeletal muscle is primarily composed of dense, regular connective tissue, similar to the tendon into which it merges.
Specimen No. 97. Urinary bladder, human, H&E Again, the transitional epithelium is located at the bottom of the section. The epithelium has multiple layers and the outer layer contains many dome-shaped cells. This allows identification as transitional epithelium, fixed when the bladder was relatively empty. The layers present are similar to what was described for Slide 95, except that the outermost layer (seen at the top of the section) is irregular and is not bounded by mesothelium. This layer is most correctly referred to as an adventitia and is characteristic of the inferior and posterior surfaces of the bladder that are attached to other pelvic organs.
Specimen No. 98. Urinary bladder, human, H&E The features of this slide are very similar to those shown in Slide 95, including fixation in distension and the presence of a serosa.
|
||
Click here to submit questions or comments about this site. Updated 05/30/21 - Velkey |
||