Cases for Week 19
Review Items for Week 2: Inflammation
Microbiology/Pathology Case Descriptions
Micro Case 1
Clinical history: Over the course of 1 week, a 6-year-old boy develops 0.5- to 1.0-cm pustules on his face. During the next 2 days, some of the pustules break, forming shallow erosions covered by a honey-colored crust. New lesions then form around the crust. The boy's 40-yearold uncle develops similar lesions after visiting for 1 week during the child's illness.
Image Gallery:
(Summary of Gross and Lab Findings - click here)
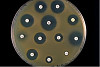
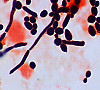
The photograph shows a particularly severe case of impetigo bullosa. It is highly contagious and frequently seen in otherwise healthy children and occasionally in adults who are in poor health. The blood agar plate shows colonied with beta hemolysis typical of Staphylococcus aureus. The organism is catalase and coagulase positive. A positive coagulase test is shown. Most organisms that cause imptetigo are antiobiotic sensitive. The technique for perfoming antiobiotic sensitivity is illustrated. Examples of antiobiotic sensitive and methicillin resistant Staph aureus are shown.
|
(Summary of Microscopic Findings - click here)
A swab taken from the lesion and gram stained shows gram positive cocci. Gram stain from the culture plate shows gram positive cocci in clusters.
|
m1-1. What is the MOST LIKELY diagnosis?
ANSWER
m1-2. The Gram stain from a skin pustule showed gram positive cocci in clusters. The organism grew on sheep blood agar (SBA) and was catalase positive. What is the most likely microorganism?
A. Staphylococcus aureus
B. Staphylococcus epidermidis
C. Streptococcus pyogenes
D. Streptococcus pneumonia
ANSWER
Case 12 (Micro Case 2)
[ImageScope] [WebScope]
Clinical History: A 65-year-old woman had experienced increasing malaise with nocturia and polyuria for the past year. Her blood pressure was 170/95. Urinalysis showed 1+ proteinuria. Serum BUN and creatinine were elevated. She developed worsening renal failure and died of pneumonia.
Image Gallery:
(Summary of Gross Findings - click here)
The kidneys are small with irregular and coarse U-shaped corticomedullary scars overlying dilated, blunt, deformed calyces. Extensive scarring is noted at the hilum of each kidney. Evidence of hydronephrosis and cortical thinning is also observed.
|
(Summary of Microscopic Findings - click here)
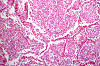
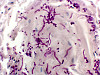
Interstitial tissue shows prominent infiltration by lymphocytes and plasma cells, and occasional polymorphonuclear neutrophils; irregular fibrous scars and peri-glomerular fibrosis. Tubules are dilated, many filled with eosinophilic casts giving the region a "thyroid-like" appearance. A few tubules contain polymorphonuclear neutrophils, indicating that this is an active exacerbation of a chronic pyelonephritis. Arteries are markedly thickened, with intimal proliferation resulting in narrowing of the lumen. Many arterioles show hyaline changes in their walls. Most glomeruli are replaced by fibrous tissue. A few are surprisingly normal in appearance with intact capillaries. There is a prominent peri-glomerular fibrosis in many regions with a thick rim of fibrous tissue circling the outside of Bowman's capsule.
|
(Review Normal Histology - click here)
Norm No. 2 Kidney
[ImageScope] [WebScope]
The kidney excretes soluble waste from the body and controls electrolyte balance. It consists of the cortex and the medulla. Within the outer cortex, glomeruli with delicate capillary loops are seen. The basement membrane is thin and without inflammation or thickening. Bowman’s capsule that surrounds the glomerulus is thin. The interstitium demonstrates no evidence of inflammation or fibrosis. In the areas between the glomeruli, tubules and arterioles are seen. The tubules are intact. The vessels exhibit no narrowing or wall thickening. The inner medulla of the kidney contains only tubules and blood vessels. Larger arteries and veins are located at the interface between cortex and medulla.
|
|
m2-1. What is the BEST diagnosis?
- Chronic glomerulonephritis
- Chronic pyelonephritis
- Arteriolonephrosclerosis
- Nodular glomerulosclerosis
- Analgesic nephropathy
ANSWER
m2-2. A child with hypertension should be studied to rule out:
- Chronic glomerulonephritis
- Arteriolonephrosclerosis
- Reflux nephropathy
- Renal artery dilatation
- Wilm’s tumor
ANSWER
Micro Case 3 (Path Slide 51)
[ImageScope] [WebScope]
Clinical History: A 45-year-old male became ill approximately 2 to 3 weeks ago following an alcoholic spree. He had nausea, vomiting, dehydration, confusion and high fever. He died suddenly shortly after admission.
Image Gallery:
(Summary of Gross and Lab Findings - click here)
Gram stain of sputum obtained before death shows Gram positive cocci in pairs. The right lung was heavy weighing 700 grams. Its lower lobe showed diffuse gray consolidation. The trachea and bronchi contained a great deal of mucus, and the mucosa was dark red.
|
(Summary of Microscopic Findings - click here)
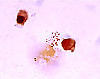
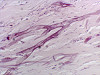
The alveoli are distended and contain a large amount of inflammatory exudate, which consists of many polymorphonuclear leukocytes, a few RBC's, macrophages and strands of fibrin. Many RBC's have been phagocytosed by the macrophages and are undergoing disintegration. The alveolar septa are delicate and well preserved, but markedly congested.
|
What is the MOST LIKELY diagnosis AND the likely causative agent?
ANSWER
m3-1. These images depict pneumonia in the stage of:
- Congestion
- Red hepatization
- Gray hepatization
- Resolution
- Abscess formation
ANSWER
m3-2. Community acquired atypical pneumonia can be caused by which of the following organisms?
- Legionella pneumophilia
- Staphylococcus aureus
- Klebsiella pneumoniae
- Mycoplasma pneumoniae
- Pseudomonas aeruginosa
ANSWER
Micro Case 4 (Path Slide 195)
[ImageScope] [WebScope]
Clinical History: A 67-year-old male had rheumatic heart disease for thirty years. Three months prior to death he began to have episodes of fever and chills accompanied by signs of worsening congestive heart failure. Splinter hemorrhages and purpuric skin rashes were noted three weeks before death.
Image Gallery:
(Summary of Gross and Lab Findings - click here)
Blood cultures grew alpha-hemolytic streptococci. Gram stain shows gram positive cocci in chains. The heart weighed 400 grams. There was thickening of the mitral valve leaflets and the chordae tendineae. Many friable calcified pink-gray granular verrucae were present on the valve. In addition, a large vegetation of the same type was found on the left auricular endocardium.
|
(Summary of Microscopic Findings - click here)
The section represents a portion of mitral valve, left atrium and left ventricle. The valve is greatly thickened and damaged. It is infiltrated with acute and chronic inflammatory cells, and shows a zone of necrosis and fibrosis in the central portion of the valve. The myocardium shows slight focal fibrosis, and focal acute inflammatory infiltration in some sections.
|
m4-1. What is the MOST LIKELY diagnosis?
ANSWER
m4-2. Most cases that present with these findings are caused by:
- Chlamydiae
- Rickettsiae
- Fungi
- Bacteria
ANSWER
m4-3. In this particular patient the MOST LIKELY causative organism was:
- Group A Streptococci
- Viridans Streptococci
- Staphylococcus aureus
- Staphylococcus epidermidis
ANSWER
m4-4. The organism MOST LIKELY to infect normal heart valves is:
- Group A Streptococci
- Group B Streptococci
- Viridans Streptococci
- Staphylococcus aureus
ANSWER
m4-5. The organism MOST OFTEN associated with infective endocarditis in IV drug abusers is:
- Group B Streptococci
- Viridans Streptococci
- Staphylococcus aureus
- Staphylococcus epidermidis
ANSWER
m4-6. The heart valve MOST OFTEN affected by infective endocarditis in IV drug abusers is the:
- Aortic valve
- Mitral valve
- Pulmonic valve
- Tricuspid valve
ANSWER
m4-7. Which of these organisms are normal flora of the throat and are associated with dental caries, brain abscesses, and endocarditis?
- Staphylococcus epidermidis
- Streptococcus viridans
- Streptococcus pneumoniae
- Peptostreptococcus species
ANSWER
m4-8. A patient with suspected infectious endocarditis has a St. Jude’s prosthetic aortic valve and a fever of 38.6C (101.5F). Blood culture shows non-hemolytic, small, white colonies. The organism was Gram positive, catalase positive and coagulase negative. What is the MOST LIKELY organism?
- Streptococcus viridans
- Streptococcus pyogenes
- Stapylococcus epidermidis
- Staphylococcus aureus
ANSWER
m4-9. A throat culture grows normal oropharyngeal flora. What alpha-hemolytic organism is most likely to be isolated on the blood agar?
A. Staphylococcus epidermidis
B. Staphylococcus viridans
C. Streptococcus pneumoniae
D. Peptostreptococcus species
ANSWER
m4-10. A throat culture grows normal oropharyngeal flora. The coagulase test for the organism is positive. What is the genus and species of the organism?
A. Staphylococcus aureus
B. Streptococcus agalactiae
C. Streptococcus pyogenes
D. Staphylococcus epidermidis
ANSWER
Micro Case 6 (Path Slide 123)
[ImageScope] [WebScope]
Clinical History: A 25 year-old woman had pelvic pain, fever, and vaginal discharge for 3 weeks. On physical examination, she has lower abdominal adnexal tenderness and a painful, swollen left knee. Laboratory studies show WBC count of 11,875/mm3 with 68% segmented neutrophils, 8% bands, 18% lymphocytes, and 6% monocytes.
Image Gallery:
(Summary of Gross and Lab Findings - click here)
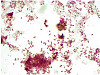
The uterine tubes were markedly distended and thickened with adhesions between the fimbriated end and the ovaries. On sectioning, pus exuded from the lumen. Cultures grown in chocolate agar and Thayer-Martin agar (TMA contains antibiotics that permit the growth of certain species) yielded colonies. The organisms were small gram negative cocci in pairs.
|
(Summary of Microscopic Findings - click here)
The villi are plump and edematous, with marked dilation and congestion of capillaries. The mucosa is heavily infiltrated by polymorphonuclear leukocytes, which have broken through foci of necrotic mucosa, producing the purulent exudate. Besides this acute phase, there are chronic features evidenced by plasma cell, lymphocytic and macrophage infiltration and fibroblastic proliferation. The muscular layers are edematous and infiltrated by acute and chronic inflammatory cells. This probably represents gonorrheal infection, the mucosa being predominantly involved, in contrast to other pyogenic infections which more frequently involve the outer layers and relatively spare the mucosa.
|
m6-1. What is the MOST LIKELY diagnosis AND the likely causative agent?
ANSWER
m6-2. What is a likely complication of this disease?
- Ectopic pregnancy
- Infertility
- Tubo-ovarian abscess
- ALL of the above
ANSWER
m6-3. What organisms are most likely to cause this disease?
- Bacteria
- Viruses
- Fungi
- Parasites
ANSWER
m6-4. Which of the following statement about this disease is FALSE?
- It is usually associated with endometriosis
- May be complicated by strictures and infertility
- May also involve the adjacent ovary
- May result in a hydrosalpinx
- May be complicated by septicemia
- ALL of the above statements are false regarding this disease.
- NONE of the above statements are false regarding this disease.
ANSWER
m6-5. The following organisms are commonly responsible for pelvic inflammatory disease EXCEPT:
- Gonococci
- Chlamydia
- Aspergillus
- Streptococcus
- Staphylococcus
ANSWER
m6-6. A 25-year-old male presents with urethritis. The Gram stain shows intracellular gram positive cocci. What is the most likely organism?
- Chlamydia trachomatis
- Ureaplasma species
- Neisseria gonorrhoeae
- Haemophilus ducreyi
ANSWER
Micro Case 7 (Path Slide 9)
[ImageScope] [WebScope]
Clinical History: A 51-year-old male had a "neurogenic bladder", caused by a spinal cord tumor. He had multiple bladder infections which were treated with antibiotics. He had surgery to remove the tumor. Postoperatively, he developed fever and costovertebral angle tenderness which did not respond to antibiotics. He expired and an autopsy was performed.
Image Gallery:
(Summary of Gross and Lab Findings - click here)
A catheterized urine specimen was obtained before death and submitted for culture studies. The organism grew on sheep blood agar (SBA) and on MacConkey agar with over 100,000 colony forming units/ml of urine. Gram stain of a blood culture showed gram negative rods. The bladder was distended, with a thickened, trabeculated wall. There was a bilateral hydroureter and hydronephrosis. The left kidney was swollen, and the cut surface showed soft foci of yellow streaks extending toward the pelvis.
|
(Summary of Microscopic Findings - click here)
Naked eye examination of the slide reveals dark streaks extending from the outer cortex to the inner medulla. Microscopically these are foci of acute inflammation, including necrosis and hemorrhage, with masses of polymorphonuclear leukocytes that are also found in many tubules.
|
m7-1. What is the BEST diagnosis?
- Acute pyelonephritis
- Acute glomerulonephritis
- Chronic pyelonephritis
- Chronic glomerulonephritis
ANSWER
m7-2. ALL of the following are risk factors for this condition EXCEPT:
- Reflux nephropathy
- Congenital vesicoureteral reflux
- Posterior urethral valves
- Acetaminophen (Paracetamol) overdose
- Urolithiasis
ANSWER
m7-3. A urine culture from an 18-year-old woman with similar symptoms also grew a pure culture of more than 100,000 colonies/ml of an organism on sheep blood agar (SBA) and MacConkey’s agar. The gram stain also showed gram negative rods. What is the most likely organism?
- Escherichia coli
- Enterococcus species
- Staphylococcus epidermidis
- Staphylococcus saprophyticus
ANSWER
Micro Case 14 (Path Slide 451)
[ImageScope] [WebScope]
Clinical History: A 4-year-old female had a gradual onset of fever, productive cough, anorexia and diarrhea about eleven days prior to death. The breath sounds were harsh, and a few cracking rales were heard over the right base posteriorly.
Image Gallery:
(Summary of Gross and Lab Findings - click here)
Sputum smear showed acid fast bacilli. Sputum cultures results became available four weeks after death, showing the presence of slow-growing colonies. The lungs showed fibrinous exudates over the pleural surfaces. The cut surface of the lung revealed innumerable small, gray-white nodules 1-4 mm in size. A large caseous tubercle of 0.5 cm was present in the left lower lobe, eroding into a large pulmonary vessel.
|
(Summary of Microscopic Findings - click here)
A lower power examination reveals numerous poorly defined tubercles approximately of the same size and same stage of development. These tubercles show a slight caseous necrosis and consist predominantly of mononuclear cells, epithelioid cells, and a few giant cells. In alveoli there is a moderate amount of mononuclear cell infiltration. Some lymphocyte and plasma cell infiltration is diffusely present in the alveolar septa.
|
m14-1. Based on these clinical findings, what is the likely causative agent?
ANSWER
m14-1. Which of the following is the BEST diagnosis?
- Ghon complex
- Miliary (disseminated) tuberculosis
- Foreign body reaction to talcum powder
- Atypical pneumonia
- H1N1 influenza
ANSWER
Micro Case 15
Clinical history: A 35-year-old man with HIV complains that he has had a "bad" taste in his mouth and discoloration of his tongue for the past 6 weeks.
Image Gallery:
(Summary of Gross and Lab Findings - click here)
There are areas of adherent, yellow-tan, circumscribed plaque on the oropharynx and the tongue. This plaque can be scraped off as a pseudomembrane to show an underlying granular, erythematous base. The material is composed of organisms and inflammatory debris. Gram stained smear shows yeast with pseudohyphae. Culture shows pearly colonies typical of yeast. Germ tube test is positive. Invasive infections may occur in immunocomprised individuals. Pseudohyphae may be seen in tissue section with PAS stain.
|
m15-1. What is the MOST LIKELY diagnosis?
ANSWER
m15-2. In a separate case, a blood culture from a neutropenic (<100 neutrophils/ul) 50-year-old woman on broad spectrum antibiotics grew a yeast. Tests for germ tubes were positive in the microbiology laboratory. What is the likely organism?
- Candida albicans
- Candida tropicalis
- Candida pseudotropicalis
- Candida parapsilosis
ANSWER
Micro Case 16
Clinical history: A 44-year-old diabetic woman developed facial pain over the past 24 hours. She has become lethargic and obtunded. There is swelling with marked tenderness over the left and right maxilla, bilateral exophthalmos, diffuse abdominal pain, poor skin turgor, and dry mucous membranes. Her temperature is 37.7°C. She has tachycardia, but no murmurs, and tachypnea; the lung fields are clear.
Image Gallery:
m16-1. What is the MOST LIKELY diagnosis and the best treatment option?
ANSWER
m16-2. In a separate case, A 22-year-old with non-Hodgkins lymphoma was profoundly neutropenic after induction chemotherapy and developed fevers. Broad spectrum IV antibiotic therapy was administered, but fevers continued. Chest x-ray showed new bilaterial fluffy pulmonary infiltrates. A bronchoscopy was performed which showed hyaline, septate hyphae with acute-angle branching. What is the MOST LIKELY organism?
- Blastomyces dermatitidis
- Mucor spp
- Candida species
- Aspergillus spp
ANSWER
Micro Case 21
Clinical history: An HIV positive male presented in clinic with confusion and disorientation. He had a fever 38.5°C and photophobia. His CD4 count was 80/ul. A lumbar puncture was performed. It showed 32 WBC/ul with 89% lymphocytes, and 6% monocytes, glucose of 22mg/dl, and protein of 89mg/dl. Gram stain showed yeast and India ink showed a thick capsule.
Image Gallery:
m21-1. Which of the following is the most likely pathogen?
- Cryptococcus neoformans
- Hemophilus infulenzae
- West Nile virus
- Streptococcus pneumoniae
ANSWER
m21-2. In a separate case, A 35-year-old man who received kidney transplantation was being treated with cyclosporine, azathioprine, and high doses of corticosteroids. While on this regimen, the patient began to experience headaches and became lethargic. A clinical diagnosis of meningoencephalitis was made. He died 7 days later. Autopsy showed a gelatinous meningeal exudate, and on sectioning of the brain, multiple small cyst-like areas were seen. Microscopic examination showed areas containing rounded structures with a prominent capsule that stained brightly with mucicarmine.
Image Gallery:

What is the most likely organism?
- Cryptococcus neoformans
- Hemophilus infulenzae
- West Nile virus
- Streptococcus pneumoniae
ANSWER
INFLAMMATION Review Items
Key Vocabulary Terms (click here to search any additional terms on Stedman's Online Medical Dictionary)
LEARNING OBJECTIVES
Absolutely critical information you must know to practice medicine is in bold font.
Important information that will be needed for routine patient care is in regular font.
Information about less common diseases that you may encounter in clinical practice and that will probably appear on examinations is in italics
- Describe vascular changes and cellular events of the inflammatory reaction.
- Discuss the five cardinal signs of inflammation in terms of pathogenesis and underlying morphologic changes.
- Discuss chemical mediators of inflammation, in terms of origin and in vivo function:
- Discuss each of the following in terms of the associated type of inflammation (acute, chronic, or granulomatous) and their role in the inflammatory response:
- Describe the steps involved in the isolation and destruction of an infectious agent by polymorphonuclear leukocytes (neutrophils). Describe important related extracellular and intracellular factors.
- Compare and contrast acute, chronic, and granulomatous inflammation in terms of:
- etiology
- pathogenesis
- histologic appearance
- laboratory findings
- characteristic cells involved
- outcome
- systemic effects
- Compare and contrast resolution, organization and termination of an inflammatory response.
|