Website cases:
Additional cases (NOT assigned):
Gross specimen videos:
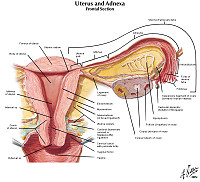
| Organ |
Diagnosis |
Video |
| Breast |
Inflammatory carcinoma |
Video |
| Breast |
Invasive ductal carcinoma |
Video |
| Ovary |
Mature teratoma |
Video |
| Uterus |
Cervical carcinoma |
Video |
| Uterus |
Endometrial carcinoma |
Video |
CASE NUMBER 506 -slide courtesy of UMich
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 14-year-old girl presented to her pediatrician with a two-month history of right-sided lower abdominal pain. She also noted that she felt “bloated." A CT scan revealed an 8-cm cystic right adnexal mass and the patient underwent a salpingo-oophorectomy. Gross and microscopic images are provided.
506-1a. What is the differential diagnosis at initial presentation?
506-1b. What is the differential diagnosis following the CT scan?
506-1c. What is the final diagnosis?
--ANSWER--
Image Gallery:
Review Ovarian Histology
Norm No. 4 Ovary
[DigitalScope]
Ovary tissue consists of stoma which is composed of elongated stromal cells. Within the stoma are oocytes in various stages of development. Most of the oocytes have not been stimulated to mature. These resting oocytes have very large nuclei with prominent nucleoli. There are corpora albicantia in a bland stroma. The Corpus Luteum of Pregnancy is composed of granulosa cells with abundant foamy cytoplasm. The granulosa cells are arranged in complex folds.
|
|
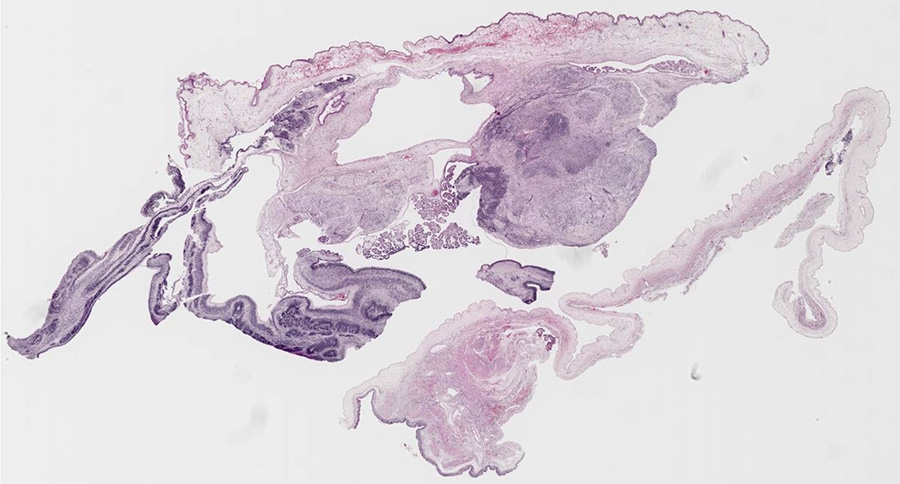
Summary of Gross Findings
The ovary is enlarged and has a heterogeneous appearance with areas of fleshy, white tissue. Focally, there is a cyst. Notably, there is no grumous, sebaceous material present.
|
Summary of Microscopic Findings
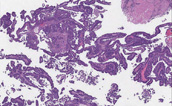
There are a variety of mature tissues, including choroid plexus (the papillary structures near the center of the tissue), and squamous epithelium (most of the top edge of the tissue). The immature component is seen best in the lower left quadrant of the slide, where there are several highly cellular “blue” areas at low power. At higher power, there are large numbers of primitive small cells with hyperchromatic nuclei, some of which are arranged in rounded “rosettes” around a central lumen-like space These are neuroblasts, and are by far the most common immature component seen in immature teratomas.
|
Gross image questions:
- Describe the gross findings.
VM image questions:
- For the VM image, take a screenshot and annotate: squamous epithelium, respiratory epithelium and immature tissue.
506-2.Which of the following features distinguishes a mature from an immature teratoma?
- 5-hydroxytryptamine production
- Abundant sebaceous material
- Brisk mitotic activity
- Necrosis
- Presence of embryonal tissue
--ANSWER--
506-3. Risk of metastasis in immature ovarian tumor is most closely correlated with which of the following?
- Amount of necrosis
- Degree of nuclear pleomorphism
- Number of mitotic figures per ten high-power fields
- Proportion of immature neuroepithelium
- Serum β-HCG levels
--ANSWER--
CASE NUMBER 199
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 54-year-old woman presented to her primary care physician with a 9-month history of a breast mass. Mammography revealed a mass with microcalcifications and a needle biopsy was performed. Based on the histologic findings, the patient subsequently underwent a simple mastectomy with sentinel lymph node biopsy.
199-1a. What is the differential diagnosis based at initial presentation?
199-1b. How does the mammogram add to your differential diagnosis?
199-1c. What is the final diagnosis?
--ANSWER--
Image Gallery:
Review Mammary Gland Histology
Norm No. 19 Mammary Gland
[DigitalScope]
The female breast is a secretory organ that produces milk during lactation. Breast tissue that is not stimulated to lactate consists of resting apocrine cells arranged in nests and small ductules which are lined by cuboidal epithelium. The secretory units are separated from one another by loose connective tissue.
|
|
Summary of Gross Findings
There is inflammation and dimpling of the areola. The cut surface of the resected breast tissue reveals a 3 x 3 x 2 cm firm mass with stellate borders. The center of the mass is firm, scirrhous and white because of the desmoplasia. There are areas of yellowish necrosis in the portions of neoplasm infiltrating into the surrounding breast. Such tumors appear very firm and non-mobile on physical exam.
|
Summary of Microscopic Findings
The virtual image was derived from a breast biopsy on another patient and shows both intraductal carcinoma with a comedo pattern of necrosis and invasive infiltrating ductal carcinoma. Ductal carcinomas range from well-differentiated tumors characterized by good duct formation to poorly-differentiated tumors. This one is composed of infiltrating glands and sheets of pleomorphic cells which infiltrate into the adjacent breast tissue. This infiltrating ductal carcinoma of breast at low magnification appears to radiate from a central area of desmoplasia. This collagenous component gives the neoplasm a hard "scirrhous" consistency that is palpable on physical examination or breast self-examination. Such an invasive carcinoma may be fixed to underlying chest wall, making it non-mobile. Also note the nerve which is invaded by tumor. It would also be important for treatment and prognosis to determine if the tumor cells were estrogen and progesterone receptor positive.
|
Radiology image questions:
- For the radiographic image, what is the significance of the calcifications?
- Which benign and malignant entities are associated with calcifications?
Gross image questions:
- Describe the gross specimen. Which benign and malignant entities would be in your differential diagnosis based on this appearance?
VM image questions:
- For the VM, take a screenshot and annotate:
- a relatively normal lobule and the 2 types of cell populations that are present
- an area of carcinoma in situ and an area of invasive carcinoma.
199-2. If the frozen section of the sentinel lymph node is positive for metastatic carcinoma, which of the following should be the next step in that patient’s therapy?
- Bilateral mastectomy and bilateral axillary lymph node dissection
- Complete axillary lymph node dissection and right mastectomy
- Intraoperative radiation of the surgical field
- Right mastectomy alone
- Stop the surgery so the patient can begin neoadjuvant chemotherapy
--ANSWER--
199-3. Which of the following correlates most strongly with a poor prognosis in this tumor?
- Dermal lymphatic involvement
- Expression of estrogen and progesterone receptors
- Low tumor stage
- Small tumor size
- Tubular carcinoma histologic type
--ANSWER--
199-4. Which of the following elements are evaluated in the staging of this tumor?
- Amount of nuclear pleomorphism
- Degree of tubule formation
- Extent of necrosis
- Presence of microcalcifications
- Tumor size
--ANSWER--
199-5. Five years later, the patient presented with a lytic bone lesion of the right femur. A PET scan shows that the lesion is extremely avid for 18F-fluorodeoxyglucose. A needle biopsy of the patient’s femur lesion showed undifferentiated carcinoma. Which of the following techniques would be the next most logical step to confirm that this is metastatic breast carcinoma?
- DNA microarray analysis
- Flow cytometry
- Fluorescent in situ hybridization
- Immunohistochemistry
- Tissue culture
--ANSWER--
CASE NUMBER 15 - slide courtesy of UMich
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 72-year-old woman presents to her gynecologist with a 1-month history of intermittent blood-tinged vaginal discharge. Her last menstrual period was 20 years earlier. Ultrasound reveals an endometrial thickness of 8 mM. A biopsy is performed.
15-1a. What is the differential diagnosis at initial presentation?
15-1b. How does the ultrasound contribute to the differential diagnosis?
15-1c. What is the final diagnosis?
--ANSWER--
Image Gallery:
Review Uterine Histology
Norm No. 21 Uterus
[DigitalScope]
The uterus is a reproductive organ, capable of enormous growth during pregnancy. It is composed of an inner endometrium which supports the placenta during pregnancy. The glandular endometrium undergoes monthly cycles in response to endocrine influence. It undergoes proliferation and then a secretory phase when it is capable of supporting a fertilized ovum. It is subsequently shed during menstruation. The endometrial here is proliferative. If you look carefully you can see mitotic figures in the endometrial glands. Note the regular spacing and orderly array of the endometrial glands. Beneath the endometrium is the myometrium which is composed of smooth muscle cells.
|
|
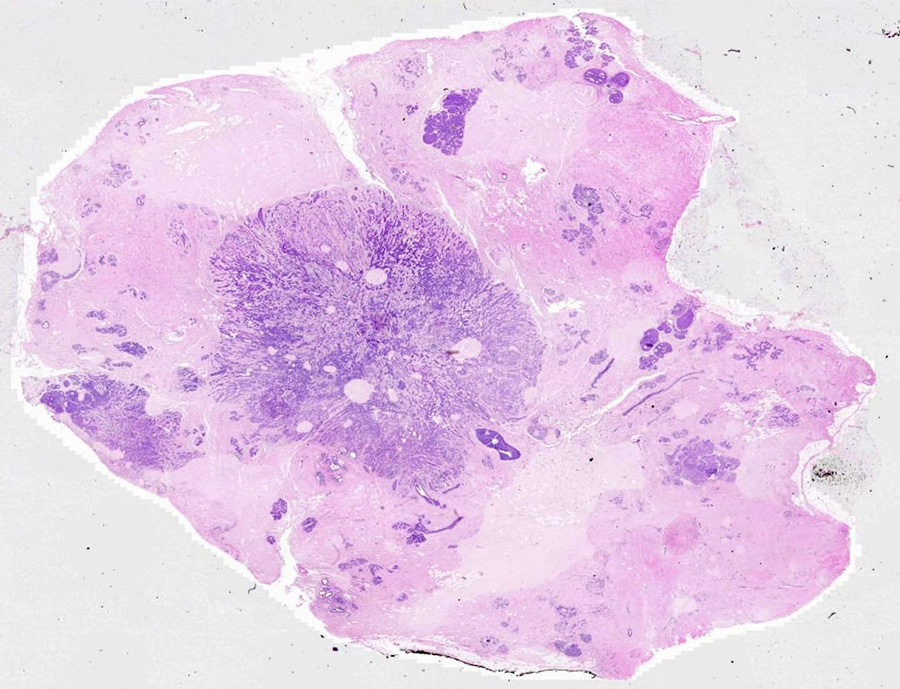
Summary of Microscopic Findings
There are fragments of tissue that show papillary architecture. The neoplastic cells show marked cytologic atypia, a high nuclear-to-cytoplasm ratio and brisk mitotic activity. There are scattered foci of necrotic cells. Psammoma bodies are not present in this section. These tumors may show glandular or solid growth patterns, in addition to papillations.
|
VM image questions:
- Describe the findings of the VM.
- Take a screenshot and annotate: an area with papillary architecture, necrosis, pleomorphism and a mitotic figure.
- Is this a high grade or low-grade lesion?
15-2. Which of the following genes is most commonly mutated in this disease?
- BRCA1
- LKB1 / STK11
- TP53
- PTEN
- RB
--ANSWER--
15-3. Which of the following is most accurate regarding this entity?
- Endometrial hyperplasia is the precursor lesion
- It is the most common endometrial malignancy
- Most tumors are low grade
- Obesity is a risk factor
- Prognosis is typicaly poor
--ANSWER--
CASE NUMBER 11
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 17-year-old girl presents to her obstetrician for her first prenatal visit at 8 weeks estimated gestational age. A transabdominal ultrasound reveals a uterus that is more appropriate for a 10-week gestation. Fetal heart sounds are not appreciated. An endovaginal ultrasound is then performed.
11-1a. What is the differential diagnosis based on initial presentation and ultrasound findings?
11-1b. What is the final diagnosis?
--ANSWER--
Image Gallery:
Summary of Ultrasound Findings
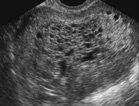
A fetus is not seen. The uterine cavity is distended by innumerable variably sized anechoic cysts with intervening echoic material.
|
Radiology image questions:
- Describe the ultrasound of the uterus.
- What would be your differential diagnosis based on these findings?
11-2. A laboratory test for serum levels of which of the following would be most appropriate at this juncture?
- α-fetoprotein
- β-HCG
- Estrogen
- Lactate dehydrogenase
- Prostacyclin
--ANSWER--
CASE NUMBER 11, PART 2 - slide courtesy of UMich
[DigitalScope]
Clinical History (continued): The appropriate test is performed and shows levels of >100,000 mIU/mL. Dilation and curettage is performed.
Image Gallery:
Review Placental Histology
Slide 253 placenta, 1st trimester DigitalScope
Slide 255 placenta, term DigitalScope
With the implantation of a zygote into the uterus, a number of changes take place in the endometrium. Cells from the embryonic trophoblast invade the uterine mucosa, secretions from these cells coalesce to form lacunae in the endometrium, which is now termed the decidua. These spaces also contain maternal blood. The trophoblast rapidly invades the decidua forming primary villi, that contain only trophoblast (outer syncytiotrophoblast and inner cytotrophoblast) cells. Mesenchyme and blood vessels form the core of the secondary villi. During the second half of pregnancy the cytotrophoblast cells disappear and the capillary basal lamina fuses with that of the syncytiotrophoblast to improve exchange.
Begin with slide 253 DigitalScope , which is early placenta. The entire field is filled with villi cut predominantly in cross section. Mesenchymal tissue and fetal blood vessels (filled with fetal RBCs which, in the early stages of fetal hematopoiesis, still have nuclei) make up the core of each villus which is covered by a trophectoderm shell of inner cytotrophoblast and outer syncytiotrophoblast cells. The syncytiotrophoblast cells are more eosinophilic and have smaller nuclei. As the name implies, these cells result from the fusion of many cells and thus have many nuclei per cell and no discernable lateral boundaries. In contrast, cytotrophoblast cells are clearly demarcated, have a single, large nucleus and basophilic cytoplasm. Notice that there is almost a complete ring of cytotrophoblast cells covering each villus in early placenta --these cells are thought to function as stem cells for the formation of the syncytiotrophoblast, which is why they may disappear later in pregnancy.
Study slide 255 DigitalScope, which is a late placenta. Although you will be able to see an occasional cytotrophoblast cell, you will not be able to see forming villi in this late placenta. Examine the trophectoderm shell, which now consists of multinucleate syncytiotrophoblast cells located on the outer surface of the villi as well as an occasional residual underlying cytotrophoblast cell. The nuclei of the syncytiotrophoblast cells often form aggregates of so-called "syncytial knots" that may look like specks of dirt when viewed at lower magnification. Syncytiotrophoblast cells that are bathed in maternal blood have apical surfaces specialized for absorption (microvilli), pinocytosis, and exocytosis and an appearance typical of secretory cells. Also examine the numerous macrophage-like (Hofbauer) cells that can be found within the connective tissue of the placental villi. These cells are characteristically large, with elliptical, eccentric nuclei and extensively vacuolated cytoplasm.
Many late or term placenta exhibit an amorphous eosinophilic fibrinoid substance, deposited in the intervillus space as shown in this older placenta. This material clings to the villus surface and may bind several villi together. The amount of fibrinoid deposition in combination with the appearance of the connective tissue in the villi can be used to stage the placenta. Although some degree of fibrinoid deposition is normal, excessive deposition can impede oxygen exchange and can cause placental failure.
|
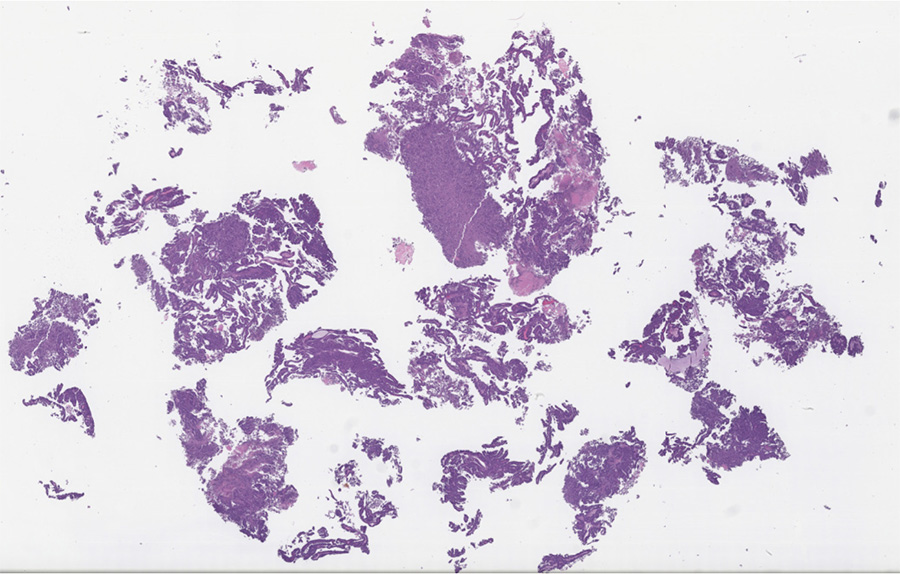
Summary of Gross Findings
The placenta is composed of masses of grape-like clusters of hydropic villi. Fetal tissue and normal placental tissue are not present.
|
Summary of Microscopic Findings
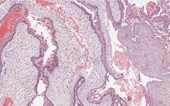
The enlarged chorionic villi are poorly vascularized and have edematous stroma with scattered “cisterns”. There is diffuse proliferation of both cytotrophoblast and syncytiotrophoblast in a circumerferential pattern. Normal villi are not present. On the left side of the slide is a portion of decidualized endometrium.
|
Gross image questions:
- Describe the gross findings of the provided specimen.
VM image questions:
- Describe the VM findings.
- Take a screenshot and identify: syncytiotrophoblast and endometrial glands and stroma.
- How does the appearance of this endometrial tissue differ from that seen in a nongravid uterus?
11-3. What is the correct diagnosis?
--ANSWER--
11-4. Which of the following is the most likely karyotype of this tissue?
- 46, XX
- 46, XY
- 46, YY
- 69, XXX
- 69, XXY
--ANSWER--
11-5. Which of the following is most commonly associated with this disease entity?
- Choriocarcinoma
- Ectopic pregnancy
- HELLP syndrome
- Obesity
- Toxoplasmosis
--ANSWER--
CASE NUMBER 123
The goal of this case is to explore how anatomic pathology findings manifest in the ways that patients present to medical attention with initial symptoms, as well as how this affects the subsequent course of disease.
We will work through a clinical case with two different clinical complications of one initial STI. Please read through the case as presented in the image gallery below (or in this document) and actively engage with the embedded questions, using the current course material to inform --ANSWER--s. Feel free to use any available resources to think through the questions. Also, students may work together in groups to discuss the cases.
Image Gallery:
After having worked through the slides above, click here for a video debrief from Dr. Alspaugh regarding the infectious disease component of this case.
Clinical History (continued): She underwent a right salpingo-oophorectomy and the resected tissue was submitted for histopathology.
123-1. What is the differential diagnosis?
--ANSWER--
Virtual microscopy slide: [DigitalScope]
Image Gallery:
Review Oviduct Histology
Norm No. 20 Uterine (fallopian) tube (aka oviduct)
[DigitalScope]
The fallopian tube is lined by ciliated columnar epithelium that aid in transport of the ovum to the uterus. The epithelium is arranged in fronds that project into the lumen. The wall consists of smooth muscle and connective tissue.
|
|
Summary of Gross Findings
The uterine tubes were markedly distended and thickened with adhesions between the fimbriated end and the ovaries. On sectioning, pus exuded from the lumen.
|
Summary of Microscopic Findings
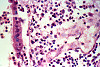
The villi are plump and edematous, with marked dilation and congestion of capillaries. The mucosa is heavily infiltrated by polymorphonuclear leukocytes, which have broken through foci of necrotic mucosa, producing the purulent exudate. Besides this acute phase, there are chronic features evidenced by plasma cell, lymphocytic and macrophage infiltration and fibroblastic proliferation. The muscular layers are edematous and infiltrated by acute and chronic inflammatory cells. This probably represents gonorrheal infection, the mucosa being predominantly involved, in contrast to other pyogenic infections which more frequently involve the outer layers and relatively spare the mucosa.
|
--Click here for a video debrief of the pathology findings presented in this case--
123-2. Which of the following is the most likely complication of this condition?
- Appendicitis
- Ectopic pregnancy
- Endometriosis
- Polycystic ovarian disease
- Preeclampsia
--ANSWER--
123-3. Which of the following is the most common etiologic agent in this condition?
- Candida albicans
- Chlamydia trachomatis
- Herpes simplex virus-2
- Mycobacterium tuberculosis
- Human papillomavirus
--ANSWER--
CASE NUMBER 220
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 58-year-old woman presented to her gynecologist with a two-year history of uterine prolapse and urinary incontinence. A hysterectomy was performed. Gross and microscopic images are provided.
220-1. What is the differential diagnosis?
--ANSWER--
Image Gallery:
Review Uterine Histology
Norm No. 21 Uterus
[DigitalScope]
The uterus is a reproductive organ, capable of enormous growth during pregnancy. It is composed of an inner endometrium which supports the placenta during pregnancy. The glandular endometrium undergoes monthly cycles in response to endocrine influence. It undergoes proliferation and then a secretory phase when it is capable of supporting a fertilized ovum. It is subsequently shed during menstruation. The endometrial here is proliferative. If you look carefully you can see mitotic figures in the endometrial glands. Note the regular spacing and orderly array of the endometrial glands. Beneath the endometrium is the myometrium which is composed of smooth muscle cells.
|
|
Summary of Gross Findings
The uterus was slightly enlarged, and contained many gray firm circumscribed nodules 0.5 cm - 2 cm in size. These nodules bulged out of the cut surface. Most of them were located intramurally, but there were some are located in the sub mucosal or the subserosal areas.
|
Summary of Microscopic Findings
The tumor nodules are composed of interlacing bundles of cells, which have long spindle nuclei and pink fibrillary cytoplasm. These cells resemble the smooth muscle cells of the myometrium. Portions of the tumor tissue have become pink hyalinized masses in which only a few cells are present. These tumor nodules do not have a definite capsule, though their outlines are rather distinct. A small number of vessels are present within the tumor.
|
220-2. Which of the following are the proliferating cells in this tumor?
- Endometrial epithelium
- Endometrial stromal cells
- Fibroblasts
- Smooth muscle cells
- Schwann cells
--ANSWER--
220-3. Which of the following is the most common presenting sign for this tumor?
- Abdominal mass
- Dyspareunia
- Menorrhagia
- Pelvic pain
- Urinary incontinence
--ANSWER--
220-4. The presence of which of the following would be most worrisome for malignancy in this tumor?
- Brisk mitotic activity
- Calcification
- Multifocality
- Pedunculation
- Subserosal location
--ANSWER--
FEMALE GENITAL SYSTEM Review Items
Key Vocabulary Terms (click here to search any additional terms on Stedman's Online Medical Dictionary)
Gynecological Pathology Learning Objectives
Goal 1: Infections of the Female Genital Tract
Apply knowledge of physiology and anatomy to compare and contrast the clinical presentation and pathology of pelvic infections.
Objective 1: Clinical Features of Pelvic Infections
Discuss the common pelvic infections including those affecting the vulva, vagina, cervix, and fallopian tubes, and describe the pathogenesis of pelvic inflammatory disease, common organisms involved, and its complications.
Goal 2: Vulva
Apply knowledge of infectious disease and principles of neoplasia to discuss the malformations and diseases of the vulva.
Objective 1: Vulvitis
Describe the etiologic factors, clinical presentation and consequences of vulvar inflammation.
Objective 2: Non-neoplastic Epithelial Disorders
Compare and contrast lichen sclerosus and lichen simplex chronicus in terms of clinical presentation, etiology, pathologic findings and disease progression.
Objective 3: Neoplasms of the Vulva
Describe the risk factors, epidemiology, pathologic findings and factors related to prognosis for neoplasms of the vulva.
Goal 3: Cervical Disorders
Apply knowledge of cervical physiology and anatomy to compare and contrast the clinical presentation and pathology of common cervical disorders.
Objective 1: Clinical Features of Cervical Dysplasia and Neoplasms
Discuss the common human papillomavirus (HPV) types that affect the cervix and discuss the pathogenesis of cervical dysplasia and neoplasia, and cervical screening methods and prevention.
Goal 4: Non-neoplastic Uterine Disorders
Apply knowledge of uterine physiology, endocrinology and anatomy to compare and contrast the clinical presentation and pathology of common non-neoplastic uterine disorders.
Objective 1: Endometrial Hyperplasia
Define endometrial hyperplasia and discuss its etiology, classification and prognosis.
Objective 2: Uterine Adenomyosis
Compare and contrast the pathology of adenomyosis with endometriosis.
Objective 3: Abnormal Uterine Bleeding
Discuss causes of abnormal uterine bleeding including hormonal disturbances, acute and chronic endometritis, and endometrial polyps.
Goal 5: Uterine Neoplasia
Apply knowledge of the molecular basis of neoplasia to describe the clinical presentation, biologic behavior, morphologic appearance, classification, diagnosis, prognosis and targeted therapy of uterine neoplasms.
Objective 1: Clinical Features of Uterine Neoplasms
Describe common uterine neoplasms, including important clinical features, and relate pathologic features to treatment and prognosis.
Objective 2: Endometrial Carcinoma
Compare and contrast the precursors, clinical setting, risk factors, pathologic findings and prognosis for type I and type II carcinomas of the endometrium.
Objective 3: Smooth-Muscle tumors of the Uterus
Define the natural history, clinical presentation and management of benign and malignant smooth muscle tumors of the uterus.
Goal 6: Ovarian Neoplasia
Apply knowledge of the principles of neoplasia to describe the clinical presentation, biologic behavior, morphologic appearance, classification, diagnosis, prognosis, and targeted therapy of ovarian neoplasms
Objective 1: Causes of Ovarian Neoplasm
Describe the risk factors, genetic associations, and molecular basis, including hereditary cancer syndromes, for ovarian neoplasms, including those derived from epithelium, sex-cord stromal as well as germ cell neoplasms.
Objective 2: Features of Ovarian Neoplasms
Compare and contrast the different types of ovarian neoplasms in terms of clinical presentation, pathologic findings, prognostic factors and treatment.
Goal 7: Polycystic Ovary Syndrome
Apply knowledge of endocrine processes to explain the clinical presentation of polycystic ovary syndrome.
Objective 1: Polycystic Ovary Syndrome
Explain the pathophysiologic basis, clinical presentation and pathologic findings of polycystic ovary syndrome.
Goal 8: Disorders of Pregnancy
Apply knowledge of embryology, cellular responses to injury, hemodynamics, and molecular alterations to summarize the clinical presentation, morphologic appearance, classification, diagnosis, biologic behavior of and therapy for disorders of pregnancy.
Objective 1: Ectopic Pregnancy
Describe risk factors, characteristic morphologic findings, potential outcomes, and the medical/surgical options for management of ectopic pregnancy in relation to the pathogenesis and likelihood of adverse consequences.
Objective 2: Infections during Pregnancy
Discuss the ascending and hematogenous infections occurring during pregnancy in terms of etiology, pathogenesis, morphology, methods of diagnosis, prognosis, and treatment.
Objective 3: Eclampsia
Explain the principal pathophysiologic aberrations of the placenta and maternal circulation in preeclampsia and eclampsia; the characteristic morphologic features in the placenta, liver, kidney, and brain; and optimal management.
Objective 4: Gestational Trophoblastic Disease
Explain with specific examples how to differentiate forms of gestational trophoblastic disease based on etiology, pathogenesis, morphologic features, clinical features, and laboratory findings, including potential consequences and/or subsequent risks, treatment, and prognosis for each.
BREAST PATHOLOGY
Key Vocabulary Terms (click here to search any additional terms on Stedman's Online Medical Dictionary)
Breast Pathology Learning Objectives
Goal 9: Non-neoplastic Disorders of the Breast
Apply knowledge of the embryology, cellular responses to injury, underlying etiology, and biologic and molecular alterations to describe the clinical presentation, inheritance risk, biologic behavior, morphologic appearance, classification, diagnosis, prognosis and therapy of non-neoplastic disorders of the breast.
Objective 1: Clinical Presentation of Breast Lesions
Identify the most frequently diagnosed breast lesions by age of the patient, based on the most common clinical presentations.
Objective 2: Reactive Breast Conditions
Compare and contrast reactive breast conditions in terms of etiology, pathogenesis, morphology and clinical features.
Objective 3: Fibrocystic Change
Discuss the clinical significance of proliferative and non-proliferative fibrocystic change, with and without atypia, and describe the subsequent risk of developing breast cancer.
Goal 10: Molecular Basis of Breast Neoplasms
Apply knowledge of the molecular basis of neoplasia to describe the clinical presentation, biologic behavior, morphologic appearance, classification, diagnosis, prognosis and targeted therapy of breast neoplasms.
Objective 1: Fibroadenoma and Phyllodes Tumor
Compare and contrast fibroadenoma and phyllodes tumor in terms of clinical features, morphologic findings, and prognosis.
Objective 2: Precursors to Breast Carcinoma
Describe the proposed precursor-carcinoma sequence in breast cancer and name the characteristic morphologic changes.
Objective 3: Ductal Carcinoma-in-Situ
Compare and contrast ductal carcinoma in situ (DCIS) and lobular carcinoma in situ (LCIS) in terms of incidence, clinical presentation, morphology, biomarker expression, pattern of spread, natural history, treatment, and prognosis.
Objective 4: Breast Cancer Susceptibility Genes
For the most common breast cancer susceptibility genes, describe the normal function of the gene product, incidence of gene mutation, reasons for its association with cancer, percent of hereditary breast cancer, and risk of breast cancer related to age.
Objective 5: Gene Expression in Breast Cancer
Explain the major molecular classes of invasive ductal carcinoma of the breast identified by gene expression profiling, and describe how each correlates with prognosis and response to therapy.
Objective 6: Categories of Breast Cancer
Compare and contrast invasive ductal carcinoma (NOS), invasive lobular carcinoma, medullary carcinoma, colloid (mucinous) carcinoma, tubular carcinoma, and inflammatory carcinoma of the breast in terms of incidence, age predilection, etiology, pathogenesis, clinical presentation, gross and microscopic morphology, grade, molecular classification, patterns of spread, clinical course, prognostic indicators, treatment options and survival rates.
Objective 7: Factors Affecting Response and Prognosis of Breast Cancer
Explain the prognosis and likelihood of recurrence and response to therapy for a breast cancer patient based on knowledge of molecular classification and/or gene expression profiling, morphologic classification, grade, prognostic marker studies, and other predictive factors.
|