|
| Readings from Robbins Basic Pathology, 11th ed |
|
| PAGES |
TOPICS |
|
| 141 - 181 |
Diseases of the Immune System (entire chapter) |
|
| 292 - 299 |
Vasculitis -through- Infectious Vasculitis |
|
| 420 |
Diffuse Pulmonary Hemorrhage Syndromes |
|
| 700 - 702 |
Rheumatoid Arthritis (w/in section on arthritis) |
|
| 184 - 5 |
Immune-Related Laboratory Tests |
|
|
|
Website Cases:
CASE NUMBER 502
[DigitalScope]
Clinical History: A 73-year-old woman presented to her primary care physician with partial vision loss in her left eye. She additionally reported a two-week history of bitemporal headaches, fatigue and weight loss. Physical exam is significant for bilateral tenderness over the temporal areas. A biopsy of the temporal artery was performed. Microscopic images are provided.
Image Gallery:
Review Blood Vessel Histology
UMich Slide 42 (mesentery, H&E) DigitalScope
UMich Slide 95M (mesentery, trichrome-elastin) DigitalScope
Slides 42 and 95M are mesentery spreads that contain numerous excellent examples small muscular arteries and their companion veins. Study the arteries first in slide #42 [example] , and/or #95 (trichrome) [example] . Note the thin intima, the distinct internal elastic lamina (IEL) and the media composed of circularly oriented smooth muscle cells. The media also contains some elastin and abundant “reticular” collagen, as well as specific proteoglycans. There is sometimes a condensation of elastic fibers in the outer portion of the media that may be an “external elastic lamina”, which varies from artery to artery. The adventitia is the dense, irregular connective tissue surrounding the media that varies in thickness. Remember that in blood vessels the components of the media are arranged circularly, while those of the adventitia are oriented longitudinally. In vessels where the media is too thick to be supported by simple diffusion, vasa vasorum (e.g. shown here in slide 95M) may also be observed in the adventitia.
The structure of the companion veins in slide #42 [example] and/or #95 (trichrome) [example] is less regular and may be difficult to understand at first, but still consists of the same basic layers as arteries with a tunica intima, media, and an adventitia, although the media is usually much less muscular and less organized compared to the companion artery. Conversely, the adventitia is usually thicker in veins and may often have some bundles of longitudinal smooth muscle [example] as well as vasa vasorum [example] . In some sections, you may be able to see a thin internal elastic lamina beneath the venular endothelium (particularly in slide #95M).
|
Physical examination of the patient's temple shows a thickened, nodular, and tender segment of the superficial temporal artery.
|
Summary of Microscopic Findings
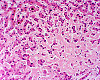
The superficial temporal artery exhibits significant thickening of the tunica intima, causing a reduction in lumenal diameter. There is extensive degradation of the internal elastic lamina as well as granulomatous inflammation consisting of an infiltrate of lymphocytes and macrophages within the tunica media. Numerous multinucleated giant cells are observed.
|
Clinical image questions
- Describe the clinical appearance.
VM image questions
- Describe the histologic findings regarding the vessel lumen, the thickness of the vessel wall and the intramural pathologic findings.
- Which type of inflammation is present?
- Which type of inflammatory cells are present
- Take a screenshot and annotate the different types of immune cells you see as well as an area of necrosis.
502-1a. What is the differential diagnosis based on the clinical history and initial presentation?
502-1b. Based on the physical exam?
502-1c. What is the differential diagnosis based on histologic findings?
--ANSWER--
502-2. Which of the following is most accurate regarding this disease?
- A negative arterial biopsy does not exclude this diagnosis
- Aortic dissection occurs in approximately 25% of patients
- Atypical B cells are the initiating stimulus
- There is a male predominance
- Vessels typically show continuous involvement
--ANSWER--
502-3. Which of the following is a rare but serious complication of this disease?
- Atrophic gastritis
- Blindness
- Hepatocellular carcinoma
- Cerebrovascular accident
- Renal failure
--ANSWER--
502-4. Which of the following arteries is most commonly affected by this disease?
- Coronary
- Pulmonary
- Renal
- Superior mesenteric
- Vertebral
--ANSWER--
CASE NUMBER 509
(no virtual slides for this case)
Clinical History: A 43-year-old woman presented to her primary care physician with a 3-month history of bilateral hand and wrist pain, stiffness and swelling. The stiffness is worse in the morning. A clinical image of her hands is provided along with a plain radiograph study. Two images that are representative of her synovium are also provided.
Laboratory tests were positive for rheumatoid factor. Over the next 25 years, she had increasing pain and deformity of her hands and also experienced pain and swelling of her feet. A plain radiograph study is provided. Two images that are representative of her synovium are provided.
Image Gallery:
Summary of Clinical Findings
First image: The hands appear symmetric. There is mild swelling in the area of the metacarpophalangeal (MCP) joints. Second image: The hands are affected symmetrically. There is subluxation of the metacarpophalangeal (MCP) joints with prominent ulnar deviation. The proximal interphalangeal (PIP) joints are also affected. There is atrophy of the interosseous muscles and prominent ulnar deviation of the fingers.
|
Summary of Radiologic Findings
The imaging studies also show subluxation of the MCP joints. In addition, there is juxta-articular osteopenia and marginal erosions in the area of the MCP joints.
|
Summary of Microscopic Findings
There is hypertrophy and hyperplasia of the synovial lining which results in a somewhat papillary architecture. There is a prominent mixed inflammatory infiltrate that includes lymphocytes and plasma cells. The vasculature is prominent (due to angiogenesis) There is a lymphoid aggregate in image 1.
|
|
Clinical image questions:
- Compare and contrast the two clinical images with descriptions of each.
--ANSWER--
Radiology questions:
- Describe the radiologic features. How do they correlate with the clinical findings?
- Which joints are predominantly involved by disease?
- Does the bone uniformly appear of normal density?
--ANSWER--
VM image questions:
- Describe the histologic findings. How would you describe the architecture of the synovium?
- Which type of inflammatory cells are present? Identify a lymphoid aggregate.
--ANSWER--
509-1a. What is the differential diagnosis based on the patient’s initial presentation?
509-1b. Based on the entire clinical history and radiologic findings?
509-1c. Based on the histologic findings?
509-1d. What is the final diagnosis and why?
--ANSWER--
509-2. Which of the following antibodies are MOST LIKELY to be demonstrated in this patient?
- Anti-citrullinated peptides
- Anti-myeloperoxidase (MPO-ANCA)
- Anti-proteinase-3 (PR3-ANCA)
- Anti-smooth muscle
- Anti-transglutaminase (anti-eTg)
--ANSWER--
509-3. Which of the following is an important mediator and therapeutic target of this disease?
- Cryoglobulin
- Platelet-derived growth factor
- Toll-like receptor
- Transthyretin
- Tumor necrosis factor
--ANSWER--
CASE NUMBER 19
[DigitalScope]
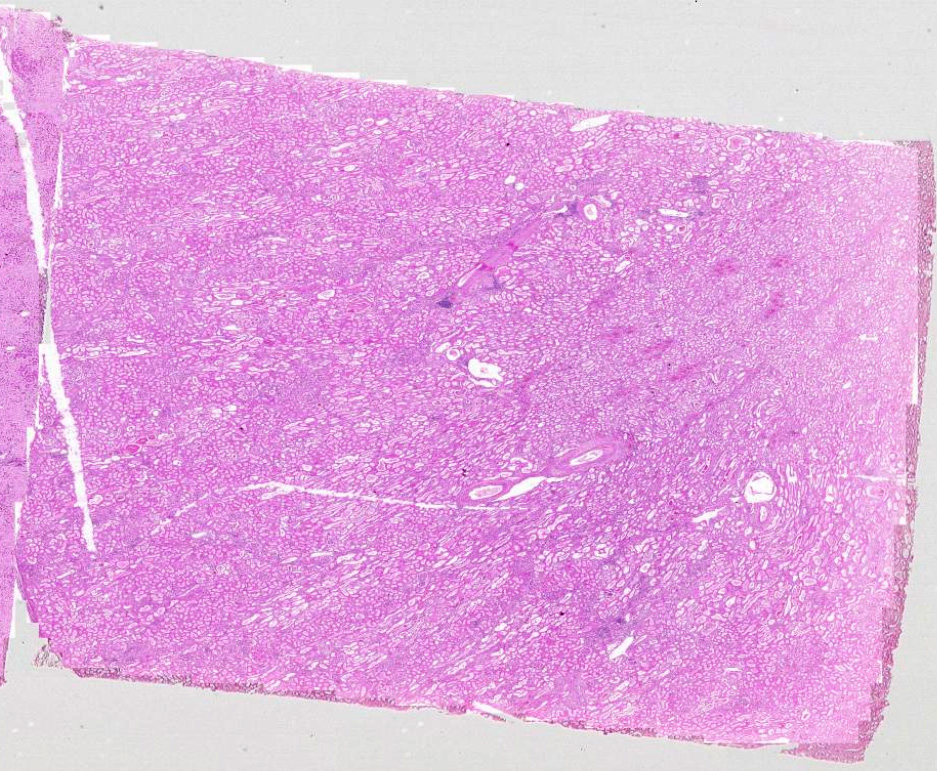
Clinical History: A 51-year-old man with a long history of tuberculosis presented to his primary care physician with a 4-week history of bilateral ankle edema. Physical examination revealed an enlarged liver and urinalysis showed 2+ proteinuria. While he was being evaluated, he experienced a ventricular arrhythmia and died. Gross and microscopic images are provided.
Image Gallery:
|
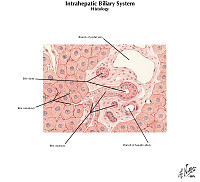
Review Liver Histology
Slide No. 3 Liver
[DigitalScope]
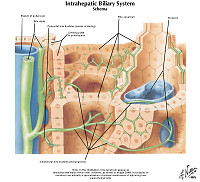
The liver is the organ that metabolizes nutrients received from the digestive tract. These nutrients and processed by tissue hepatocytes which are large polygonal cells. The hepatocyes are separated by portal triads. The triads consist of an artery, a vein and a bile duct. The bile duct is lined by cuboidal epithelium. The artery has a muscular wall and a flat endothelial lining. The sinuses are well defined and contain a small amount of blood.
|
|
Review Kidney Histology
Slide No. 2 kidney
[DigitalScope]
Slide 240 kidney
[DigitalScope]
The kidney excretes soluble waste from the body and controls electrolyte balance. It consists of the cortex and the medulla. Within the outer cortex, glomeruli with delicate capillary loops are seen. The basement membrane is thin and without inflammation or thickening. Bowman’s capsule that surrounds the glomerulus is thin. The interstitium demonstrates no evidence of inflammation or fibrosis. In the areas between the glomeruli, tubules and arterioles are seen. The tubules are intact. The vessels exhibit no narrowing or wall thickening. The inner medulla of the kidney contains only tubules and blood vessels. Larger arteries and veins are located at the interface between cortex and medulla.
|
Summary of Gross Findings
Both kidneys were large, each weighing 250 grams. This chronic renal disease may actually increase the size of the kidney. Pale deposits of amyloid are present in the cortex, most prominently at the upper center. The liver weighed 1900 grams and was firm with a waxy appearance. The heart (not shown) was also large, weighing 470 grams.
|
Summary of Microscopic Findings
Liver: Most of the liver is replaced by homogenous, hyaline pink-staining amyloid which has been laid down between the sinusoids and the liver cells. This would stain with Congo red, or would be metachromatic if stained with crystal violet. The liver cords are replaced or compressed, and appear as widely separated thin cords of cuboidal cells. Bile plugs are present in the bile capillaries.
Kidney: The same type of hyaline pink material is present in the glomeruli, and is deposited between the endothelial cells and the basement membrane. In some places, it may be present in masses that encroach on the lumen of the capillary. The amyloid can also be recognized in the walls of some small arteries, and in a few places can be seen around the tubules in the interstitial tissue.
|
|
Gross image questions:
- Screen shot and describe the findings you see in the liver specimen and your differential given the changes in the liver.
- In the image of the kidney, similarly, describe your observations and your differential based on the gross changes in the kidney, including annotations of the following:
- renal cortex,
- renal medulla, and
- abnormal areas you observe
VM image questions:
- Screen shot and annotate the liver sections highlighting:
- a portal area,
- central vein,
- areas you see which appear abnormal, providing your differential for these abnormal areas.
- In the kidney section, annotate:
- a glomerulus, tubule(s), and an area of interstitium,
- blood vessel,
- abnormal glomerular mesangial matrix, and
- abnormal arterioles. For the latter findings, describe your differential diagnosis.
19-1a. What is the differential diagnosis based on the patient’s initial presentation?
19-1b. Based on physical exam and laboratory findings?
19-1c. What is the final diagnosis and why?
--ANSWER--
19-2.The development of this particular disease in this patient is MOST LIKELY due to deposition of which of the following?
- A β-amyloid (Aβ)
- Amyloid light chain protein (AL)
- Amyloid-associated fibril (AA)
- β2-microglobulin
- Transthyretin
--ANSWER--
19-3. Which of the following stains is most commonly used to visualize the deposited substance?
- Congo red
- Oil Red O
- Periodic acid-Schiff
- Silver
- Warthin-Starry
--ANSWER--
19-4. Which of the following is the MOST COMMON cause of this disease?
- Familial Mediterranean fever
- Hemodialysis
- Plasma cell dyscrasia
- Rheumatoid arthritis
- Tuberculosis
--ANSWER--
CASE NUMBER 8
(no virtual slide for this case)
Clinical History: A 12-year-old boy with end-stage renal failure due to congenital ureteral obstruction received a living-donor renal transplant from his grandfather which failed eight years later due to noncompliance with immunosuppressive medications. At age 25, he received a second, deceased-donor renal transplant. His immunosuppressive regimen included tacrolimus (FK 506), azathioprine, and prednisone. His serum creatinine level fell during the first week post-transplant to almost normal levels, but then began to rise again, reaching a level of 5 mg/dL. A percutaneous renal biopsy was performed.
Image Gallery:
Review Kidney Histology
Slide No. 2 kidney
[DigitalScope]
Slide 240 kidney
[DigitalScope]
The kidney excretes soluble waste from the body and controls electrolyte balance. It consists of the cortex and the medulla. Within the outer cortex, glomeruli with delicate capillary loops are seen. The basement membrane is thin and without inflammation or thickening. Bowman’s capsule that surrounds the glomerulus is thin. The interstitium demonstrates no evidence of inflammation or fibrosis. In the areas between the glomeruli, tubules and arterioles are seen. The tubules are intact. The vessels exhibit no narrowing or wall thickening. The inner medulla of the kidney contains only tubules and blood vessels. Larger arteries and veins are located at the interface between cortex and medulla.
|
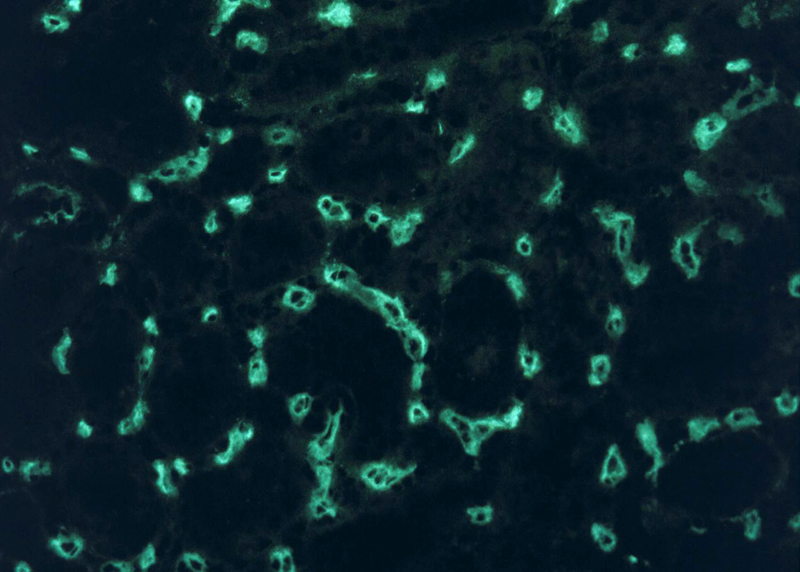
Summary of Microscopic Findings
The first two images, of H&E-stained sections, show renal tissue with a dense interstitial inflammatory infiltrate composed primarily of mononuclear inflammatory cells with occasional admixed neutrophils. A glomerulus is present in the first image and unremarkable in appearance, and tubules are largely spared by the inflammation, which seems to be centered on peritubular capillaries (located between the tubules and largely obscured by the inflammation). The final image, an immunofluorescent stain for the complement split product C4d, shows intense linear staining of peritubular capillaries. The staining pattern is due to a type II hypersensitivity reaction, which is typically linear (as opposed to type III, which is granular). The dark, non-staining areas between the capillaries are tubules.
|
VM image questions
- Using a screen shot, annotate the different compartments of the kidney (glomerulus, tubules, and interstitium).
- What is being stained using the C4d immunofluorescence?
8-1a. Based on the clinical history, what is the differential diagnosis for the patient’s rising serum creatinine?
8-1b. Based on the histologic and immunohistochemical studies, what is the final diagnosis and why?
--ANSWER--
8-2. Which of the following would be the best test to confirm the diagnosis?
- Complete blood count with differential
- Evaluation of serum complement levels
- Examination of a peripheral blood smear
- Immunohistochemical stains for cytomegalovirus
- Screening for donor-specific antibodies
--ANSWER--
Clinical History (continued): Circulating antibodies against both class I and class II histocompatibility antigens were detected by serologic testing; one of the anti-class I antibodies was donor-specific.
8-3. Which of the following is the most likely cause of anti-HLA antibodies in this patient?
- Autoimmunity
- Immune reaction to drug-bound self proteins
- Immunization by cross-reacting gut flora
- Production of anti-graft antibody by neoplastic plasma cell clone
- Sensitization by previous allograft
--ANSWER--
8-4. This patient is at greatest risk for developing which of the following?
- Graft-versus-host disease
- Hyper-IgM syndrome
- IgA deficiency
- Non-Hodgkin lymphoma
- Wiskott-Aldrich syndrome
--ANSWER--
IMMUNOPATHOLOGY Review Items
Key Vocabulary Terms
LEARNING OBJECTIVES
Goal 1: Immune Dysfunction
Apply knowledge of basic mechanisms of immunology to explain how dysfunction can produce cellular injury, acute and chronic inflammation, autoimmunity, allergic reactions, and susceptibility to infection; how these changes affect organ function and the health of the organism; and how therapeutic intervention can mitigate these effects.
- Objective 1: Innate and Adaptive Immunity
Compare and contrast innate and adaptive immunity with respect to the molecules and cells involved in the immune response, and the role of these systems in host defense.
- Objective 2: Cell Types
Compare and contrast the roles played by T cells, B cells, NK cells, macrophages and dendritic cells in the immune response.
- Objective 3: Cytokines
Discuss, with examples, the production of different cytokines by different immune cells, the roles that cytokines play in effecting the immune response, and how knowledge of cytokine action can be exploited in treatment of disease.
- Objective 4: Hypersensitivity
Compare and contrast the mechanisms of the four different hypersensitivity reactions with respect to the situations in which each is triggered, the cells and mediators involved, the resulting pathologic effects on tissue and the ultimate clinical consequences.
- Objective 5: Immune Tolerance
Define immunological tolerance, and describe the role that failure of tolerance plays in the development of autoimmune diseases.
- Objective 6: Autoimmune diseases
Compare and contrast the etiology, laboratory findings, morphologic features and clinical presentation of the various autoimmune diseases, including rheumatoid arthritis, systemic lupus erythematosus, Sjogren syndrome, systemic sclerosis, IG4-related disease, granulomatosis with polyangiitis, and the vasculitides.
- Objective 7: HLA
Discuss the structure and function of human histocompatibility antigens and describe the role of this system in both transplantation and in susceptibility to certain diseases.
- Objective 8: Transplantation
Discuss consequences of tissue transplantation, including mechanisms and pathophysiology of organ rejection (hyperacute, acute and chronic), and the possible therapeutic interventions that can mitigate these effects.
- Objective 9: Immunodeficiencies
Compare and contrast the genetic basis and inheritance patterns of the well- defined primary immunodeficiencies; discuss the mechanisms of the pathologic and clinical sequelae of these disorders; and describe therapeutic interventions that can mitigate or correct them.
- Objective 10: Secondary Immune Deficiencies
Describe the etiology, mechanisms of action and possible clinical consequences of secondary immune deficiencies.
|
Click here to submit questions or comments about this site.
|
|