Website cases:
CASE NUMBER 221
(no virtual slide for this case)
Clinical History: A 62-year-old man underwent total nephrectomy for renal cell carcinoma and subsequently received adjuvant chemotherapy. While on chemotherapy, he became leukopenic and thrombocytopenic. He presented to his oncologist with a 3-day history of a rash on his left side.
221-1. What is the differential diagnosis?
Image Gallery:
There is a band-like papulovesicular rash with lesions averaging 3-5 mm in size.
|
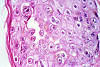
The epidermis shows spongiosis, vesicle formation, necrosis and ulceration. The epidermal cells have degrees of ballooning degeneration. Many intranuclear eosinophilic inclusion bodies are seen in these cells. Many keratinocytes within the vesicle also have multiple nuclei with nuclear "molding" and marginated chromatin. The upper dermis beneath a vesicle shows necrosis with little or no inflammatory reaction.
|
(Review Skin Histology)
Norm No. 15 Skin
[ImageScope] [WebScope]
Skin consists of keratinizing stratified squamous epithelium. The keratin layer is eosinophilic. Nuclei are not present. Beneath the keratin layer is a layer of flat epithelial cells with small pyknotic nuclei. Cells are regular and not crowded. These keratinocytes rest upon a layer of basal epithelium and a thin basement membrane. Beneath the epidermis is the dermis which consists of loose connective tissue. Within the dermis are sweat and sebaceous glands. Some slides contain hair follicles. There is no inflammation. The blood vessels are patent and do not contain thromboemboli.
|
Physical exam questions:
- Describe the rash seen on the patient’s side.
Microscopy still image questions:
On an annotated screenshot of the microscopy images on the website identify:
1) the epidermis and dermis
2) areas of the epidermis that display necrosis; and
3) features supportive of viral cytopathic change.
Differential Diagnosis questions:
221-1a. What is the differential diagnosis based on the clinical history and physical exam?
221-1b. What is the final diagnosis and why?
221-2. Which of the following is the etiologic agent for this disease?
- Cytomegalovirus
- Herpes simplex virus-2
- Human papilloma virus, type 6
- Poliovirus
- Varicella-zoster virus
221-3. Where is latent infection established following primary infection?
- Dorsal root ganglia
- Motor axons
- Neuromuscular junction
- Peripheral sensory nerves
- Skeletal muscle
221-4. Which of the following is a rare complication that can be seen in this disease?
- B-cell lymphoma
- Facial hemiparesis
- Myocarditis
- Toxic shock syndrome
- Vegetations on heart valves
CASE NUMBER 544
(no virtual slide for this case)
Clinical History: A 5-year-old boy is brought to the pediatrician because his parents notice that he walks on his toes and has difficulty climbing stairs. They state that he did not begin walking until he was 18 months old. Physical exam reveals bilaterally enlarged calves. A muscle biopsy is performed.
Differential Diagnosis questions:
544-1a. What is the differential diagnosis based on the patient’s initial presentation?
544-1b. What is the differential diagnosis following physical exam?
Image Gallery:
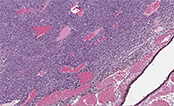
The low power view (left) shows fatty replacement of muscle fibers and hypertrophy and atrophy of fibers. The higher power view (right) shows marked fibrosis, fiber splitting, degeneration/myophagocytosis, and regeneration (internal nuclei).
|
Review Skeletal Muscle Histology
Norm No. 18 Skeletal muscle
[DigitalScope]
Skeletal muscle fibers have striations which are easily seen on the longitudinal section. Nuclei are located at the periphery of normal striated muscle fibers.
|
Microscopy still image questions:
- Describe the findings of the muscle biopsy.
- Which features are supportive of abnormal muscle histology?
- What does the immunohistochemical stain tell you about the diagnosis?
Clinical History, part 2 (click here to move on to part 2)
CASE NUMBER 523, part 1- slide courtesy of UMich
[DigitalScope]
Clinical History: An 18-year-old man presents for his Army physical. The doctor notices multiple skin lesions distributed evenly across his body and irregular areas of hyperpigmentation. The patient states that he has had these lesions his entire life but that they had never bothered him. One of the lesions is biopsied.
Differential Diagnosis questions:
523-1a. What is the differential diagnosis based on the physical exam?
523-1b. What is the final diagnosis and why?
Image Gallery:
There are multiple soft, fleshy, pedunculated lesions present. In addition, there is a focus of hyperpigmentation consistent with a café au lait spot.
|
There is an infiltrative, non-circumscribed lesion present in the dermis that is composed of wavy or buckled spindle cells distributed amidst ropy collagen bundles and myxoid stroma. Mitotic activity, necrosis and cryptologic atypia are not seen |
Review Skin Histology
Norm No. 15 Skin
[DigitalScope]
Skin consists of keratinizing stratified squamous epithelium. The keratin layer is eosinophilic. Nuclei are not present. Beneath the keratin layer is a layer of flat epithelial cells with small pyknotic nuclei. Cells are regular and not crowded. These keratinocytes rest upon a layer of basal epithelium and a thin basement membrane. Beneath the epidermis is the dermis which consists of loose connective tissue. Within the dermis are sweat and sebaceous glands. Some slides contain hair follicles. There is no inflammation. The blood vessels are patent and do not contain thromboemboli.
|
Physical exam image questions:
- Describe the skin lesions shown in the two clinical images.
- What is your differential diagnosis based on these lesions?
VM image questions:
- Describe the virtual microscopic image.
- What shape are the cells?
- Is the process circumscribed or infiltrative?
- Do you see mitotic figures?
- Is this likely benign or malignant?
523-2. A mutation in a gene encoding which of the following is most commonly observed in patients with this disease?
- Dystrophin
- E-cadherin
- Merlin
- Neurofibromin
- Tuberin
523-3. Identification of which of the following is highly suggestive of this diagnosis?
- Hemangioblastoma
- Meningioma
- Plexiform neurofibroma
- Solitary cutaneous neurofibroma
- Vestibular schwannoma
CASE NUMBER 523, part 2- slide courtesy of UMich
[DigitalScope]
Clinical History (continued): Ten years later, the patient presents to his primary care physician with a 3-week history of “burning” and “shooting” nerve pain in his right arm. MRI revealed a 5 cm mass within the brachial plexus. The mass was excised.
Differential Diagnosis questions:
523-4a. What is the differential diagnosis based on the patient’s current presentation?
523-4b. What is the differential diagnosis with the addition of the imaging studies?
523-4c. What is the final diagnosis and why?
Image Gallery:
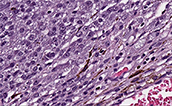
Residual neurofibroma is present on the superior aspect of the tissue. The remaining tissue shows fascicular architecture, cytologic atypia, hypercellularity and scattered mitotic figures. There is focal necrosis and vascular invasion.
|
Review Skin Histology
Norm No. 15 Skin
[DigitalScope]
Skin consists of keratinizing stratified squamous epithelium. The keratin layer is eosinophilic. Nuclei are not present. Beneath the keratin layer is a layer of flat epithelial cells with small pyknotic nuclei. Cells are regular and not crowded. These keratinocytes rest upon a layer of basal epithelium and a thin basement membrane. Beneath the epidermis is the dermis which consists of loose connective tissue. Within the dermis are sweat and sebaceous glands. Some slides contain hair follicles. There is no inflammation. The blood vessels are patent and do not contain thromboemboli.
|
VM image questions:
- Describe the microscopic image. How does this microscopic section compare to the earlier biopsy?
- Find a mitotic figure and annotate (don’t spend more than 10 minutes looking!).
- Is there necrosis? How great is your concern that this is malignant? Why?
523-5. Which of the following is the life-time risk for developing this type of tumor in a patient with this disease?
- <1%
- 1 – 10%
- 21 - 30%
- 51 - 60%
- >90%
CASE NUMBER 390- slide courtesy of UMich
[DigitalScope]
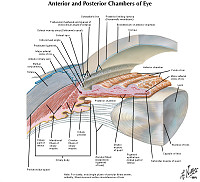
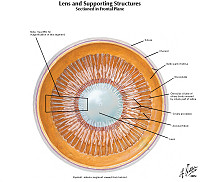
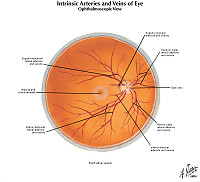
Clinical History: A 58-year-old man presented to his primary care physician with a 3-month history of blurred vision in his left eye. Previously, he had 20-20 vision in both eyes and had not seen an ophthalmologist since he was in college. A fundoscopic exam is performed.
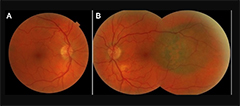
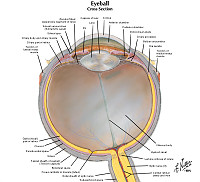
Ultrasonographic examination confirmed a diameter of 10 mm with a thickness of 3.5 mm. Following discussion, treatment options including radiation therapy and enucleation were discussed, but the patient declined. Ten months later, he presented with worsening vision and eye pain and fundoscopic exam revealed that the lesion had progressed. At this point, the patient agreed to enucleation.
Image Gallery:
There is a pigmented lesion near the fovea of the left eye.
|
There is a tumor mass within the globe of the eye. The lesion is cellular, composed of spindled to epithelioid cells. There are scattered foci of melanin pigment. The cells have large nucleoli, a classic feature in melanoma. Mitotic figures are hard to find. No necrosis is present.
|
|
|
Fundoscopy image questions:
- Describe the findings on the fundoscopic exam.
- Take a screenshot and annotate the lesion, the optic disk and the fovea for each eye.
- What would your differential diagnosis be based on the fundoscopic exam?
VM image questions:
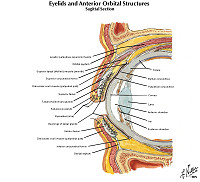
- Take a screenshot of the VM slide and annotate the following components of the retina:
- the inner limiting membrane,
- inner plexiform layer,
- inner nuclear layer,
- outer plexiform layer and
- outer nuclear layer (the outer segments of the rods and cones are a bit hard to see, so also indicate where they WOULD be).
- Describe the lesion. Identify an area with spindle cells and an area with epithelioid cells. Identify melanin pigment.
Differential Diagnosis questions:
390-1a. What is the differential diagnosis based on the patient’s initial presentation?
390-1b. What is the differential diagnosis following the fundoscopic exam?
390-1c. What is the final diagnosis and why?
390-2. Which oncogene is most commonly mutated in this disease?
- BAP1
- CFH
- GNAQ
- RHO
- USH2A
390-3. Which feature is associated with worse prognosis in this disease?
- Depth of invasion
- Lateral extent of tumor
- Origination in the iris
- Spindle cell morphology
- Ulceration
390-4. Which of the following is the most common site of metastasis for this tumor?
- Bone
- Brain
- Liver
- Lung
- Soft tissue
MUSCLE PATHOLOGY Review Items
Muscle Pathology Key Vocabulary Terms (click here to search any additional terms on Stedman's Online Medical Dictionary)
Eye Pathology Key Vocabulary Terms (click here to search any additional terms on Stedman's Online Medical Dictionary)
PNS: GOALS and LEARNING OBJECTIVES
Goal: Neuromuscular and Muscular Disorders
Apply knowledge of clinical, anatomic and neuropathologic principles to the diagnosis of neuromuscular and muscular disorders.
- Objective 1: Amyotrophic Lateral Sclerosis
Describe the etiology, pathogenesis, and clinical features of amyotrophic lateral sclerosis.
- Objective 2: Mitochondrial Disorders
Describe the etiology, pathogenesis, and clinical features of mitochondrial diseases affecting muscle.
- Objective 3: Muscular Dystrophies
Compare and contrast the etiology, pathogenesis, and clinical features of the dystrophiopathies.
- Objective 4: Acquired Disorders of Skeletal Muscle
Compare and contrast the etiology, pathogenesis, and clinical features of inflammatory myopathies and toxic myopathies.
Goal: Pathology of Peripheral Nerves
Apply knowledge of clinical, anatomic and neuropathologic principles to the diagnosis of neural disorders.
- Objective 1: Disorders Associated with Peripheral Nerve Injury
Compare and contrast the peripheral neuropathies in terms of etiology, risk factors, clinical presentation, pathologic findings and natural history.
- Objective 2: Disorders of the Neuromuscular Junction
Compare and contrast the disorders of the neuromuscular junction in terms of etiology, risk factors, clinical presentation, pathologic findings and natural history.
- Objective 3: Peripheral Nerve Sheath Tumors
Compare and contrast benign and malignant tumors of the peripheral nerve sheath in terms of etiology, genetics, associated syndromes, clinical presentation, pathologic findings and prognostic factors.
|