CASE NUMBER 370 - slide courtesy of UMich, luxol blue stain
[ImageScope] [WebScope]
Clinical History: A 67-year-old woman with a long history of hypertension and a remote myocardial infarction presented to the emergency department with a two-hour history of left-sided weakness. She reported that she had a “fluttering” sensation in her chest and that her cardiologist had recommended treatment for atrial fibrillation which she had refused. While in the emergency department, she developed left-sided hemiparesis. She was admitted to the hospital for observation; however, her condition worsened and she went into a coma. She died 17 days after admission.
Image Gallery:
(Summary of Gross Findings - click here)
There was thrombosis of the right internal carotid artery just above the bifurcation. There was extensive necrosis of the right frontal, parietal and temporal lobes and basal ganglia.
|
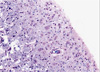
(Summary of Microscopic Findings - click here)
This is a luxol stain, which stains cell bodies (most abundant in the cortex) light pink whereas myelin (most abundant in the white matter) is dark blue. There is an area of liquefactive necrosis in which many macrophages with phagocytosed fat and myelin particles are present. At the pial surface and within the white matter surrounding the necrotic area are numerous large astrocytes (reactive gliosis) with large vesicular nuclei and abundant eosinophilic cytoplasm. The myelin in this area stains pale (compared to more healthy white matter seen on the right side of the slide) due to surrounding edema fluid. The blood vessels are congested and there is some extravasated blood. (H&E stain)
|
(Review Normal Histology - click here)
Cerebrum
Slide 76 (cerebrum, luxol blue/cresyl violet) [WebScope] [ImageScope]
Slide 76b (toluidine blue & eosin) [WebScope] [ImageScope]
The cerebral cortex is loosely stratified into layers containing scattered nuclei of both neurons and glial cells. Examine the layered organization of the cerebral cortex using slide 76 stained with luxol blue/cresyl violet [ORIENTATION] (which stains white matter tracts and cell bodies) or toluidine blue and eosin [ORIENTATION] (TB&E, toluidine blue stains the nuclei and RER of cells whereas eosin stains membranes and axon tracts). Typically one or more sulci (infoldings) will extend inward from one edge of the section. Examine the gray matter on each side of the sulcus using first low and then high power. Neurons of the cerebral cortex are of varying shapes and sizes, but the most obvious are pyramidal cells. As the name implies, the cell body is shaped somewhat like a pyramid, with a large, branching dendrite extending from the apex of the pyramid toward the cortical surface, and with an axon extending downward from the base of the pyramid. In addition to pyramidal cells, other nuclei seen in these sections may belong to other neurons or to glial cells also present in the cortex. You may be able to see subtle differences in the distribution of cell types in rather loosely demarcated layers. There are 6 classically recognized layers of the cortex:
- Outer plexiform (molecular) layer: sparse neurons and glia
- Outer granular layer: small pyramidal and stellate neurons
- Outer pyramidal layer: moderate sized pyramidal neurons (should be able to see these in either luxol blue [example] or TB&E-stained [example] sections)
- Inner granular layer: densely packed stellate neurons (usually the numerous processes aren’t visible, but there are lots of nuclei reflecting the cell density)
- Ganglionic or inner pyramidal layer: large pyramidal neurons (should be able to see these in either luxol blue [example] or TB&E-stained [example] sections)
- Multiform cell layer: mixture of small pyramidal and stellate neurons
Pyramidal cells in layers III and V tend to be larger because their axons contribute to efferent projections that extend to other regions of the CNS –pyramidal neurons in layer V of motor cortices send projections all the way down to motor neurons in the spinal cord!
Deep to the gray matter of the cerebral cortex is the white matter that conveys myelinated fibers between different parts of the cortex and other regions of the CNS. Be sure you identify the white matter in both luxol blue [example] and TB&E-stained [example] sections, as it will appear differently in these two stains. Review the organization of gray and white matter in cerebral cortex vs. spinal cord.
|
370-1. What is the differential diagnosis?
ANSWER
370-2. Which of the following is the cause of the majority of thrombotic occlusions?
- Atherosclerosis
- Bacterial endocarditis
- Bone marrow embolization
- Infectious vasculitis
- Polyarteritis nodosa
ANSWER
370-3. Which of the following microscopic features is seen in the brain 12 to 24 hours after an acute hypoxic event?
- Abundant phagocytic cells
- Central chromatolysis
- Cystic change
- Reactive astrocytosis
- Red neurons
ANSWER
370-4. Which of the following mechanisms explains the connection between atrial fibrillation and brain infarction?
- Association with Libman-Sacks disease
- Deformation of red blood cells causes vascular occlusions
- Increased incidence of nonbacterial thrombotic endocarditis
- Mural thrombi due to non-laminar flow
- Intracranial vasospasm due to decreased oxygenation
ANSWER
CASE NUMBER 504
(no virtual slide for this case)
Clinical History: A 25-year-old woman presented to her primary care physician with a one-week history of blurred vision in her left eye. She stated that it was painful to move that eye. She grew up in Minnesota and has smoked one-half of a pack of cigarettes/day for the last 7 years. Further questioning reveals that she had unilateral tingling on her left side in the two weeks before her wedding 3 years ago. CSF analysis showed mildly elevated protein and moderate pleocytosis. MRI revealed multiple hypointense lesions and FLAIR (fluid-attenuated inversion recovery) MRI showed multiple supratentorial lesions. When the patient learned of her possible diagnosis, she returned home and took an overdose of sleeping pills.
Imaging: MRI shows multiple white matter lesions in the corpus callosum, subcortical U-fibers, temporal lobes, brainstem, cerebellum and spinal cord.
Image Gallery:
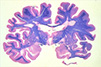
(Summary of Gross Findings - click here)
There were multiple well circumscribed somewhat depressed lesions in the white matter. A coronal section through the cerebrum has been stained with luxol fast blue/hematoxylin and eosin which stains the myelinated white matter blue and the cortex pink. There are multiple plaques of demyelination.
|
(Summary of Microscopic Findings - click here)
A high power microscopic image of white matter stained with luxol fast blue illustrates absence of myelin. The adjacent image stained with Glees silver stain illustrates that individual axons are intact.
|
|
504-1. What is the differential diagnosis?
ANSWER
504-2. The lesions in this disease are caused by an immune response directed against which of the following?
- Amyloid precursor protein
- Aquaporins
- Huntingtin
- Myelin sheath
- Substantia nigra
ANSWER
504-3. The patient has an identical twin. Which of the following most closely approximates her risk for developing the same disease?
- <1%
- 25%
- 50%
- 66%
- 75%
- 100%
ANSWER
504-4. Which of the following is typically seen in the CSF of patients with this disease?
- Abundant red blood cells
- Decreased protein level
- Myelin
- Oligoclonal bands
- PrPsc
ANSWER
NERVOUS SYSTEM PATHOLOGY Review Items
Key Vocabulary Terms (click here to search any additional terms on Stedman's Online Medical Dictionary)
LEARNING OBJECTIVES
- Absolutely critical information you must know to practice medicine is in bold font.
- Important information that will be needed for routine patient care is in regular font.
- Information about less common diseases that you may encounter in clinical practice and that will probably appear on examinations is in italics
- Describe the morphology and function of the following CNS cells:
|
|
|
- choroid plexus epithelial cells
|
|
|
|
|
- Compare CNS myelin with PNS myelin, in terms of:
- cells of elaboration
- structure and function
- reactions to injury and destruction
- regenerative potential
- Discuss normal CSF in terms of:
- sites of formation
- circulation patterns
- sites of absorption
- pressure
- glucose and protein levels
- cell types present
- Describe the blood-brain barrier (BBB) in terms of:
- physiologic definition
- anatomic counterparts
- morphologic alterations
- areas of absence
- Describe the morphology and function of the following CNS cells:
|
|
|
|
|
|
- ischemic neuronal necrosis
|
|
|
|
|
|
- Compare and contrast the following types of cerebral edema and their significance:
- cytotoxic
- vasogenic
- interstitial
- Compare and contrast the clinical findings and sequelae of herniation of the brain:
- subfalcine (cingulate gyrus)
- transtentorial (uncal)
- foraminal (tonsillar)
- Correlate destructive lesions in specific areas of the CNS with corresponding functional consequences.
- Compare and contrast:
- communicating hydrocephalus
- non-communicating hydrocephalus
- hydrocephalus ex vacuo
- Describe the following congenital abnormalities and their clinical phenotype:
|
- spina bifida/meningomyelocele
|
- Chiari type I malformation
|
|
- Chiari type II (Arnold-Chiari) malformation
|
|
- Dandy-Walker malformation
|
|
|
- agenesis of corpus callosum
|
|
|
|
|
- Compare and contrast genetics, clinical presentation and pathology of inborn errors of metabolism:
|
- spina bifida/meningomyelocele
|
- Chiari type I malformation
|
|
- Chiari type II (Arnold-Chiari) malformation
|
|
- Dandy-Walker malformation
|
|
|
- agenesis of corpus callosum
|
|
|
|
|
- Describe the effects of hypoxia/ischemia on the late gestational/perinatal brain, including the pathophysiologic mechanisms underlying the following:
|
|
- germinal matrix hemorrhage
|
|
- periventricular leukomalacia
|
|
- Discuss the clinical and pathologic features of the following processes:
- Compare and contrast the clinical and pathologic features of CNS aneurysms:
- saccular ("berry"
- atherosclerotic
- Charcot-Bouchard
- mycotic
- Compare and contrast the clinical and pathologic features of CNS vascular malformations:
- arteriovenous malformation
- cavernous angioma
- capillary telangiectasia
- List the ways in which hypertension may harm the brain.
- Compare and contrast the clinical and pathologic features of:
- hypertensive encephalopathy
- hypoxic encephalopathy
- multi infarct dementia
- Compare and contrast the clinical and pathologic features of CNS infarcts:
- nonhemorrhagic (pale, anemic)
- hemorrhagic (red)
- border zone (watershed)
- incomplete
- spinal cord
- Compare and contrast clinical presentations of infarcts in these vascular territories:
- middle cerebral
- vertebrobasilar
- internal carotid
- Describe the interrelationship between hypotension and watershed infarcts.
- Explain the basis of the reperfusion theory of causation of hemorrhagic cerebral infarcts.
- Compare and contrast the clinical and pathologic features:
- skull fracture
- parencymal brain injury
- vascular brain injury
- Compare and contrast open vs. closed head injury, complications and prognosis.
- Compare and contrast the clinical and pathologic features of the following entities:
- pyogenic meningitis
- tuberculous/mycobacterial meningoencephalitis
- viral meningoencephalitis
- fungal meningitis
- neurosyphilis
- neuroborreliosis (Lyme disease)
- rickettsial infection
- protozoal infection
- List the common bacterial agents of acute pyogenic meningitis, and the age group that each most frequently affects.
- Compare and contrast the clinical and pathologic features:
- brain abscess
- subdural empyema
- extradural abscess
- Compare and contrast the clinical and pathologic features of viral meningoencephalitis:
- arboviral encephalitides
- herpes simplex viral encephalitis
- varicella-zoster viral encephalitis
- cytomegalovirus (CMV) encephalitis
- poliomyelitis
- rabies
- human immunodeficiency virus (HIV) infections
- HIV meningoencephalitis (subacute encephalitis)
- vacuolar myelopathy
- progressive multifocal leukoencephalopathy (PML)
- subacute sclerosing panencephalitis (SSPE)
- Discuss the clinical and pathologic features of the following prion diseases:
- Creutzfeldt-Jakob disease (CJD)
- variant CJD (vCJD, "mad cow" disease)
- kuru
- scrapie
- Compare and contrast the clinical and pathologic features degenerative diseases:
|
- olivopontocerebellar atrophy
|
|
|
|
- spinocerebellar degeneration
|
- progressive supranuclear palsy
|
- amyotrophic lateral sclerosis (ALS)
|
- corticobasal degeneration
|
|
- striatonigral degeneration
|
|
|
|
- Describe multiple sclerosis (MS) in terms of:
- geographic distribution
- etiology
- age at onset
- distribution of lesions
- morphology
- clinical course
- Discuss the following nervous system disorders:
|
- carbon monoxide poisoning
|
- acute ethanol intoxication
|
|
|
- central pontine myelinolysis (CPM)
|
|
|
- Discuss the clinical and pathologic features of the following nutritional disorders:
- Wernicke encephalopathy
- Korsakoff psychosis
- neuropathic beriberi
- subacute combined degeneration
- Explain the concepts of benign vs. malignant neoplasms of the CNS.
- Compare and contrast the clinical, pathologic, epidemiologic and genetic features of the following CNS neoplasms:
- colloid cyst of third ventricle
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- malignant peripheral nerve sheath tumor
|
|
|
- Compare and contrast the clinical, pathologic and genetic features of the following phakomatoses:
|
|
|
|
|
- von Hippel-Lindau syndrome
|
- Discuss the clinical and pathologic features of the following disorders of the PNS:
|
|
|
|
|
- paraproteinemia-associated neuropathy
|
|
|
- AIDS-associated peripheral neuropathy
|
|
- hereditary motor & sensory neuropathy (HMSN)
|
|
- type I [Charcot-Marie-Tooth disease (CMT) 1]
|
|
- type III (Dejerine-Sottas disease)
|
|
|