Website Cases:
Additional cases (NOT assigned):
CASE NUMBER 18 - slide courtesy of the University of Leeds
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: An 8-year-old boy presented to his pediatrician with a sore throat and “flu-like” symptoms. A gross image of his oral cavity is shown as are culture specimens and a gram stain of organisms scraped from his tonsils.
18-1. What is the differential diagnosis?
--ANSWER--
Image Gallery:
Summary of Lab & Gross Findings
A photograph of the pharynx at initial presentation shows enlarged erythematous tonsils which are covered with purulent material. A throat culture was obtained by swabbing the pharynx. The material was then swabbed onto a blood agar plate and incubated at 37 degrees overnight. Beta hemolysis typical of Streptococcus pyogenes is shown. A gram stained smear of the culture shows gram-positive cocci in chains.
|
Clinical image questions:
- Describe the oral exam findings.
- Describe the appearance of the culture plate. Which process is occurring here?
- How would you classify the organisms from the tonsillar scrape?
Clinical History (continued): Two weeks later, the boy returned to his pediatrician and his mother reported that his urine appeared dark and that he had been urinating less frequently than usual. Physical exam showed periorbital edema and blood pressure of 200/120 mm Hg. Urinalysis revealed hematuria with red blood cell casts, and moderate proteinuria. His BUN was 180 mg/dL (normal 7-21 mg/dL). A biopsy of his kidney is shown below.
Review Renal Histology
Norm No. 2 Kidney (needle biopsy)
[WebScope] 204_HISTO_40X - Kidney (axial section)
[WebScope]
The kidney excretes soluble waste from the body and controls electrolyte balance. It consists of the cortex and the medulla. Within the outer cortex, glomeruli with delicate capillary loops are seen. The basement membrane is thin and without inflammation or thickening. Bowman’s capsule that surrounds the glomerulus is thin. The interstitium demonstrates no evidence of inflammation or fibrosis. In the areas between the glomeruli, tubules and arterioles are seen. The tubules are intact. The vessels exhibit no narrowing or wall thickening. The inner medulla of the kidney contains only tubules and blood vessels. Larger arteries and veins are located at the interface between cortex and medulla.
|
|
Summary of Microscopic Findings
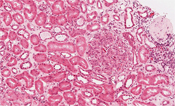
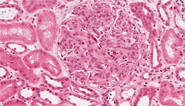
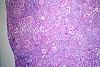
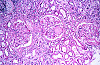
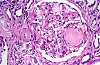
The glomeruli in this biopsy (with the exception of a few globally sclerotic ones) are diffusely, globally hypercellular (i.e., all segments of all of them are synchronously involved). They have a lobulated appearance (often described as “lobular accentuation”), and contain abundant neutrophils, but show no evidence of necrosis or crescent formation (signs of more severe, irreversible glomerular damage). There are a few small foci of interstitial inflammation (mostly associated with sclerotic glomeruli), and rare tubules contain collections of erythrocytes (presumably extravasated from inflamed glomerular capillaries and the source of the patient’s hematuria). Arteries and arterioles are unremarkable.
|
VM image questions:
- Describe the histologic findings in terms of the four compartments: glomeruli, interstitium, tubules and vasculature.
- Characterize the glomerular process as to whether it is diffuse/focal, global/segmental.
- Which types of inflammation are present in the biopsy and where?
18-2. What is now the differential diagnosis?
--ANSWER--
18-3. Which of the following is the most appropriate term for the clinical complex of 1) hematuria; 2) oliguria and azotemia; and 3) hypertension?
- Hemolytic uremic syndrome
- Malignant hypertension
- Nephritic syndrome
- Nephrotic syndrome
- Thrombotic thrombocytopenic purpura
--ANSWER--
18-4. Which of the following is a characteristic finding in patients with this disease?
- Diffuse thickening of the capillary wall
- Linear deposits of IgG
- Mesangial deposition of IgA
- Subepithelial “humps” seen on electron microscopy
- “Tram track” appearance of the glomerular basement membrane
--ANSWER--
CASE NUMBER 9
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 51-year-old man with longstanding diabetes presented to his primary care physician with a 3-week history of urinary frequency and incontinence. He reported that he had had multiple urinary tract infections over the previous year that had been treated with antibiotics. Urinalysis was positive for WBCs and bacteria. Physical exam revealed mild bilateral lower extremity weakness. A screening CT scan showed a small spinal cord tumor at T11 and the patient underwent surgery; however, postoperatively he developed fever and costovertebral angle tenderness that did not respond to antibiotics. He died on post-operative day 3. A catheterized urine specimen was obtained before death. Culture showed colonies on blood agar and on MacConkey agar. Gram stain of a blood culture showed Gram-negative rods.
9-1. What is the differential diagnosis?
--ANSWER--
Image Gallery:
Review Renal Histology
Norm No. 2 Kidney (needle biopsy)
[WebScope] 204_HISTO_40X - Kidney (axial section)
[WebScope]
The kidney excretes soluble waste from the body and controls electrolyte balance. It consists of the cortex and the medulla. Within the outer cortex, glomeruli with delicate capillary loops are seen. The basement membrane is thin and without inflammation or thickening. Bowman’s capsule that surrounds the glomerulus is thin. The interstitium demonstrates no evidence of inflammation or fibrosis. In the areas between the glomeruli, tubules and arterioles are seen. The tubules are intact. The vessels exhibit no narrowing or wall thickening. The inner medulla of the kidney contains only tubules and blood vessels. Larger arteries and veins are located at the interface between cortex and medulla.
|
|
Summary of Gross Findings
The bladder was distended, with a thickened, trabeculated wall. There was bilateral hydroureter and hydronephrosis. The left kidney was swollen, and the cut surface showed soft foci of yellow streaks extending toward the pelvis.
|
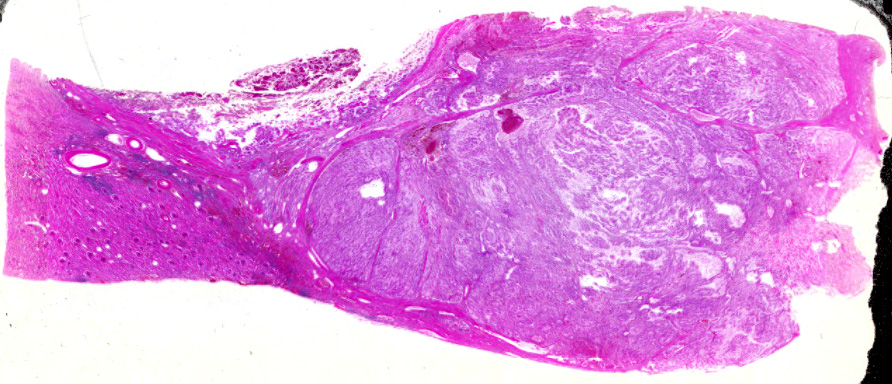
Summary of Microscopic Findings
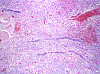
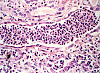
Naked eye examination of the slide reveals dark streaks extending from the outer cortex to the inner medulla. Microscopically these are foci of acute inflammation, including necrosis and hemorrhage, with masses of polymorphonuclear leukocytes that are also found in many tubules.
|
Gross image questions:
- On the gross specimen, identify the hilum of the kidney.
- Describe the gross findings of the specimen.
VM image questions:
- For the VM, take a screenshot and annotate the renal medulla, the renal cortex, an area of necrosis, an intravascular thrombus, and areas of disease.
- What is the pathologic process occurring here?
9-2. Which of the following is the most common causative organism in this disease?
- Adenovirus
- Escherichia coli
- Mycobacterium tuberculosis
- Staphylococcus aureus
- Streptococcus pneumoniae
--ANSWER--
9-3. Which of the following is the most common etiology of this disease in young children?
- Arterionephrosclerosis
- Autoantibodies to ADAMTS 13
- Gout
- Shiga toxin
- Vesicoureteral reflux
--ANSWER--
9-4. In the context of this disease, papillary necrosis is most closely linked with which of the following?
- Alcohol abuse
- Diabetes
- Male sex
- Neurogenic bladder
- Smoking
--ANSWER--
CASE NUMBER 2
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 45-year-old man presented to his general practitioner with a two-week history of right-sided flank pain. Urinalysis showed hematuria. A CT with contrast was performed. Gross and microscopic images from the nephrectomy specimen are provided.
2-1. What is the differential diagnosis?
--ANSWER--
Image Gallery:
Review Renal Histology
Norm No. 2 Kidney (needle biopsy)
[WebScope] 204_HISTO_40X - Kidney (axial section)
[WebScope]
The kidney excretes soluble waste from the body and controls electrolyte balance. It consists of the cortex and the medulla. Within the outer cortex, glomeruli with delicate capillary loops are seen. The basement membrane is thin and without inflammation or thickening. Bowman’s capsule that surrounds the glomerulus is thin. The interstitium demonstrates no evidence of inflammation or fibrosis. In the areas between the glomeruli, tubules and arterioles are seen. The tubules are intact. The vessels exhibit no narrowing or wall thickening. The inner medulla of the kidney contains only tubules and blood vessels. Larger arteries and veins are located at the interface between cortex and medulla.
|
|
Summary of Gross Findings
There is a large yellow tan tumor with areas of hemorrhage in the superior pole of the kidney. The tumor invades the renal vein and the perinephric adipose tissue.
|
Summary of Microscopic Findings
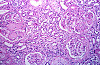
The capsule is revealed to be actually a pseudo capsule formed by compression of surrounding renal parenchyma. The tumor is made up mainly of large irregular cells, some with granular cytoplasm, and others with large vacuoles. The nuclei vary in size and shape. Some are pyknotic and some are displaced to the periphery of the large vacuolated cells characteristic of this disease.
|
Radiology image questions:
- For the CT image, take a screenshot and annotate the lesion, the aorta and the inferior vena cava.
- Describe the lesion. What would you expect the gross appearance to show?
Gross image questions:
- For the gross image, describe the lesion.
- What accounts for the yellow coloration of the mass?
VM image questions:
- For the VM image, take a screenshot and annotate areas of hemorrhage and necrosis.
- Describe the histologic findings. Are the cells pleomorphic?
2-2. Which of the following risk factors is most closely linked to the development of this disease?
- Chronic alcohol use disorder
- Diabetes mellitus
- Mutations in the PKHD1 gene
- Tobacco abuse
- Vitamin D deficiency
--ANSWER--
2-3. Which of the following is most closely associated with this disease?
- Alport syndrome
- Diabetes
- Polycystic kidney disease
- Tuberous sclerosis
- Von Hippel-Lindau disease
--ANSWER--
2-4. Which of the following extra-renal effects is most commonly associated with this entity?
- Cushing syndrome
- Dermatomyositis
- Hypoglycemia
- Polycythemia
- Trousseau syndrome
--ANSWER--
CASE NUMBER 20
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 15-year old girl presented to her pediatrician with a two-week history of frequent urination, increased thirst and weight loss. Following evaluation, she was diagnosed with insulin-dependent diabetes and was maintained on insulin therapy. Five years later, she developed proteinuria and, at the age of 45, required hemodialysis. At the age of 50, she developed pneumonia following a below knee amputation and died. Gross and microscopic images from the autopsy are provided.
20-1. What is the differential diagnosis?
--ANSWER--
Image Gallery:
Review Renal Histology
Norm No. 2 Kidney (needle biopsy)
[WebScope] 204_HISTO_40X - Kidney (axial section)
[WebScope]
The kidney excretes soluble waste from the body and controls electrolyte balance. It consists of the cortex and the medulla. Within the outer cortex, glomeruli with delicate capillary loops are seen. The basement membrane is thin and without inflammation or thickening. Bowman’s capsule that surrounds the glomerulus is thin. The interstitium demonstrates no evidence of inflammation or fibrosis. In the areas between the glomeruli, tubules and arterioles are seen. The tubules are intact. The vessels exhibit no narrowing or wall thickening. The inner medulla of the kidney contains only tubules and blood vessels. Larger arteries and veins are located at the interface between cortex and medulla.
|
|
Summary of Gross Findings
The kidneys were small and each weighed 100 grams. The surface was irregular with pits and small cysts. (image courtesy of VA Commonwealth University)
|
Summary of Microscopic Findings
There are glomerular lesions consisting of diffuse and nodular glomeroslerosis. Nodular glomerulosclerosis or Kimmelstiel-Wilson lesions are ball-like deposits of PAS positive material which contain trapped mesangial cells. These occur in 15-30% of long time diabetics and are virtually pathognomonic of the disease. Diffuse glomeruloslerosis usually appears as global sclerosis of the glomerular tuft. Chronic pyelonephritis, arterio and arteriolo nephrosclerosis as seen here are also typical findings in diabetic kidneys.
|
Gross image questions:
- For the gross specimen, describe the gross findings.
- Are the kidneys normal in size?
VM image questions:
- For the VM, describe the histologic findings in terms of the glomeruli, interstitium, tubules and vasculature.
- Take a screenshot and annotate nodular glomerulosclerosis (Kimmelstiel Wilson nodule), a sclerotic glomerulus and arteriolosclerosis.
20-2. Which of the following is the most prominent glomerular lesion in this patient?
- Crescentic proliferation of parietal epithelial cells
- Subepithelial deposits
- Mesangial IgA deposits
- Nodular glomerulosclerosis
- Subendothelial deposits
--ANSWER--
20-3. Basement membrane thickening in the eye and kidney is believed to occur through which one of the following processes?
- Activation of protein kinase C
- Disturbance in the polyol pathway
- Excess glutathione due to increased NADPH
- Decreased production of vascular endothelial growth factor
- Protein crosslinking mediated by advanced glycation end productions
--ANSWER--
20-4. Which of the following is the most common cause of end stage renal disease?
- Analgesic nephropathy
- Diabetes mellitus
- Hypertension
- Polycystic kidney disease
- Systemic lupus erythematosus
--ANSWER--
CASE NUMBER 607
(no virtual slides for this case)
Clinical History: A 45-year old man comes to the emergency department in obvious pain. He states that he has severe pain in his left flank that extends down to his left groin. The pain is sharp and intense, and it started two hours earlier.
607-1. What is the differential diagnosis?
--ANSWER--
607-2. Which of the following tests would be the best choice to help guide treatment at this point?
- Abdominal X-ray
- Chest X-ray
- EKG
- Intravenous pyelogram
- Low dose CT
--ANSWER--
Clinical History, part 2 (click here to open):
CASE NUMBER 13
(no virtual slides for this case)
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 57-year-old man presented to his primary care physician after an episode of painless hematuria. Cystoscopy was performed and a mass was noted near the dome of the bladder. The lesion was biopsied and microscopic images are provided.
13-1. What is the differential diagnosis?
--ANSWER--
Image Gallery
Review Bladder Histology
Webslide 0098_G: Urinary Bladder, monkey, H&E
[Aperio WebScope]
Note the epithelial type and the thick muscular walls. Can you find any nerves in the walls of the bladder? At high magnification examine the layer of epithelial cells next to the lumen. Large surface cells bulge into the lumen, showing jagged, scalloped edges (like a choppy seascape) indicative of the rough texture of this surface.
|
Summary of Gross Findings
Two papillary lesions are seen.
|
Summary of Microscopic Findings
The lesion shows papillary architecture with delicate fibrovascular cores surfaced by hyperplastic urothelial mucosa. The mildly atypical urothelial cells show loss of polarity with random distribution of cells in the urothelium. Perpendicular orientation to the basement membrane is also lost. Mitotic figures and marked cytologic atypia are not seen.
|
13-2. Which of the following is the most significant risk factor in the development of this lesion?
- Benzene exposure
- Bladder stones
- Cigarette smoking
- Schistosomiasis
- VHL mutation
--ANSWER--
13-3. A 35-year-old woman from Angola presents to her primary care physician following an episode of painless hematuria. A routine blood test revealed eosinophilia and subsequent ELISA analysis confirmed a diagnosis of schistosomiasis. This patient is at greatest risk for developing which of the following?
- Adenocarcinoma
- Papilloma
- Papillary urothelial carcinoma
- Small cell carcinoma
- Squamous cell carcinoma
--ANSWER--
RENAL PATHOLOGY Review Items
Key Vocabulary Terms (click here to search any additional terms on Stedman's Online Medical Dictionary)
Week 14: Kidney and Bladder LEARNING OBJECTIVES
Goal 1: Renal Syndromes
Apply knowledge of the structure and function of the kidney to describe the pathogenetic mechanisms, diagnostic criteria and clinicopathologic features of glomerular diseases presenting with asymptomatic proteinuria, nephrotic and nephritic syndrome.
Objective 1: Nephritic Syndrome
Describe the proliferative and pro-inflammatory pathologies of conditions presenting with nephritic syndrome.
Objective 2: Nephrotic Syndrome
Describe the pathophysiology and morphologic features of nephrotic syndrome.
Objective 3: Immune-mediated Renal Disease
Compare and contrast the mechanisms of immune complex- and antibody-mediated glomerulonephritis.
Objective 4: Diabetic Nephropathy
Describe the pathogenesis of diabetic nephropathy and the associated clinicopathologic features.
Goal 2: Structure and Function of the Nephron
Apply knowledge of kidney structure and function to summarize how acquired and hereditary abnormalities of the renal tubules and interstitium cause acute and/or chronic renal dysfunction.
Objective 1: Tubulointerstitial Diseases
Describe the clinicopathological features and pathogenesis of tubulointerstitial diseases and discuss how their pathogenesis relates to treatment and outcomes.
Objective 2: Nephritis
Compare and contrast acute pyelonephritis, drug-induced interstitial nephritis, and lupus nephritis in terms of pathogenesis, clinical presentation, histopathological appearance, and treatment.
Objective 3: Acute Tubular Injury
Compare and contrast ischemic and nephrotoxic forms of acute tubular injury, including typical clinical contexts, pathogenesis of renal failure, microscopic appearance, and expected outcome.
Goal 3: Renal Vascular Dysfunction
Compare and contrast the common causes of renal vascular dysfunction in terms of size and type of vessel involved, characteristic gross and microscopic morphology, pathogenesis, and clinical presentation.
Objective 1: Renal Artery Occlusion
Compare thrombotic and embolic causes of renal arterial occlusions in terms of underlying pathogenesis, gross and microscopic pathological anatomy and clinical presentation.
Objective 2: Renal Changes in Hypertension
Discuss how the pathogenesis of hypertension leads to structural changes in the renal vasculature and how the characteristic pathological vascular lesions of the kidney seen in hypertension cause renal dysfunction.
Objective 3: HUS and TTP
Compare and contrast typical hemolytic uremic syndrome (HUS), atypical HUS, and thrombotic thrombocytopenic purpura (TTP) in terms of clinical presentation, renal histopathology, pathogenesis, and prognosis.
Goal 4: Congenital Disorders of the kidney
Apply knowledge of the embryologic principles of kidney and lower urinary tract development to explain developmental anomalies.
Objective 1: Inherited Renal Disorders
Compare and contrast autosomal dominant and autosomal recessive polycystic kidney disease in terms of pathological anatomy, molecular pathogenesis, and clinical presentation.
Goal 5: Urinary Obstruction
Apply knowledge of the anatomy and physiology of the kidney to describe how disorders may lead to obstruction of urinary outflow.
Objective 1: Nephrolithiasis
List the different chemical types of nephrolithiasis, and explain the pathophysiologic mechanisms related to development, and therapy/prevention of urinary stones.
Objective 1: Causes of Urinary Obstruction
Explain several causes of urinary obstruction.
Goal 6: Renal Neoplasia
Apply knowledge of the molecular basis of neoplasia to explain the clinical presentation, biologic behavior, morphologic appearance, classification, diagnosis, prognosis and targeted therapy of renal neoplasms.
Objective 1: Renal Cell Carcinoma
Compare and contrast the 3 major types of renal cell carcinoma (clear cell, papillary, and chromophobe) in terms of clinical presentation, diagnostic morphological features, and molecular pathogenesis.
Objective 2: Urothelial and Renal-cell Carcinoma
Compare pelvic urothelial malignancies with renal cell carcinomas in relation to risk factors, microscopic appearance, and biological behavior.
Objective 3: Grading and Staging of Renal Carcinoma
Describe how renal cell carcinoma is graded and staged and discuss what determines prognosis.
Objective 4: Wilms Tumor
Describe the clinical and pathologic features and molecular basis for Wilms tumor and list the histologic features that are important to recognize in determining prognosis.
Goal 7: Bladder Infection
Apply knowledge of innate and adaptive immunity, pathogenic organisms infecting the bladder and their transmission to explain the natural history, pathogenesis, diagnosis, laboratory profiles, histopathological features, and prevention of cystitis.
Objective 1: Cystitis
Recognize the typical clinical symptomatology of the different types of cystitis.
Goal 8: Bladder Neoplasia
Apply knowledge of the molecular basis of neoplasia to describe the clinical presentation, biologic behavior, morphologic appearance, classification, diagnosis, prognosis and targeted therapy of bladder neoplasms.
Objective 1: Urothelial Carcinoma
Compare and contrast the different precursor lesions of urothelial carcinoma in terms of architecture, cytologic features, molecular-genetic changes, and propensity for invasion/progression.
Objective 2: Risk Factors for Urothelial Carcinoma
Relate the risk factors for urothelial carcinoma to general principles of carcinogenesis.
Objective 3: Staging of Bladder cancer
Relate stage of bladder cancer to prognosis and therapy, including the role of BCG, in treatment of low-stage tumors.
|