|
| Readings from Robbins Basic Pathol, 10th ed. |
by TUESDAY |
by THURSDAY |
|
| |
pages |
topics |
pages |
topics |
|
| Lab Sections 1, 2, and 3 |
pp 364 - 382 |
Blood Pressure - Noninfectious Vasculitis |
pp 97 - 101 |
Hyperemia - Hemostasis |
|
| |
|
|
pp 106 - 119 |
Thrombosis - Stages of Shock |
|
| |
|
|
pp 485 - 492 |
Bleeding Disorders - Coag Disorders |
|
| |
|
|
handout |
|
|
| |
|
|
|
|
|
| Lab Sections 4 and 5 |
pp 97 - 101 |
Hyperemia - Hemostasis |
pp 364 - 382 |
Blood Pressure - Noninfectious Vasculitis |
|
| |
pp 106 - 119 |
Thrombosis - Stages of Shock |
|
|
|
| |
pp 485 - 492 |
Bleeding Disorders - Coag Disorders |
|
|
|
| |
handout |
|
|
|
|
|
|
CASE NUMBER 4 (UMich slide 12)
[ImageScope] [WebScope]
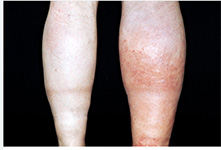
Clinical History: A 44-year-old woman (BMI = 32) with a longstanding history of uncontrolled type II diabetes presents to the emergency department with a 1-week history of worsening left foot pain.
On exam: BP 150/92, HR 97, RR 18, O2 98% on room air. Cardiovascular exam shows a regular rate and rhythm. Lungs are clear to auscultation bilaterally. Abdomen is soft, nontender. There is trace bilateral edema with loss of hair on the shins. Image of toes of left foot is shown below.
Image Gallery:
(Summary of Clinical Findings - click here)
The second and third toes show gangrenous necrosis: coagulative necrosis of multiple tissue layers. This is due to ischemia secondary to advanced atherosclerosis of the medium-sized arteries of the lower extremities.
|
4-1a. Based on the findings thus far, what is the differential diagnosis?
ANSWER
Clinical History (continued): Laboratory tests were performed with the following results:
CBC and BMP are unremarkable.
Hemoglobin A1c: 10%
Fasting blood glucose: 250 mg/dL
Total cholesterol: 304 mg/dL
LDL cholesterol: 210 mg/dL
HDL cholesterol: 28 mg/dL
Triglycerides: 300 mg/dL
The patient was admitted to the hospital, given IV antibiotics, and a left below knee amputation is scheduled. Unfortunately, she expires during the procedure.
Image Gallery:
(Summary of Gross Findings - click here)
Cross sections of the left anterior descending coronary artery demonstrate marked atherosclerosis with narrowing, more pronounced in the more proximal portion of this artery. In general, the worst atherosclerosis is proximal, where arterial blood flow is more turbulent. More focal lesions mean that angioplasty or bypass can be more useful procedures.
|
(Summary of Microscopic Findings - click here)
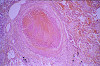
Approximately 2/3 of the original lumen is filled with atherosclerotic plaque characterized by foam cells (macrophages that are filled with cholesterol. There are areas of cholesterol clefts that consist of extracellular cholesterol. The lipids are extracted during tissue processing, leaving large empty spaces. Calcification is also present as amorphous deposits of basophilic debris. This is dystrophic calcification which, as you will recall, is associated with areas of necrosis.
|
(Review Normal Histology - click here)
Muscular Arteries and Veins
UMich Slide 42 (mesentery, H&E) WebScope ImageScope
UMich Slide 95M (mesentery, trichrome-elastin) WebScope ImageScope
Slides 42 and 95M are mesentery spreads that contain numerous excellent examples small muscular arteries and their companion veins. Study the arteries first in slide #42 [example] , and/or #95 (trichrome) [example] . Note the thin intima, the distinct internal elastic lamina (IEL) and the media composed of circularly oriented smooth muscle cells. The media also contains some elastin and abundant “reticular” collagen, as well as specific proteoglycans. There is sometimes a condensation of elastic fibers in the outer portion of the media that may be an “external elastic lamina”, which varies from artery to artery. The adventitia is the dense, irregular connective tissue surrounding the media that varies in thickness. Remember that in blood vessels the components of the media are arranged circularly, while those of the adventitia are oriented longitudinally. In vessels where the media is too thick to be supported by simple diffusion, vasa vasorum (e.g. shown here in slide 95M) may also be observed in the adventitia.
The structure of the companion veins in slide #42 [example] and/or #95 (trichrome) [example] is less regular and may be difficult to understand at first, but still consists of the same basic layers as arteries with a tunica intima, media, and an adventitia, although the media is usually much less muscular and less organized compared to the companion artery. Conversely, the adventitia is usually thicker in veins and may often have some bundles of longitudinal smooth muscle [example] as well as vasa vasorum [example] . In some sections, you may be able to see a thin internal elastic lamina beneath the venular endothelium (particularly in slide #95M).
|
4-1b. Based on these additional findings, what is the differential diagnosis?
ANSWER
4-2. List 5 risk factors for the development of atherosclerosis:
ANSWER
4-3. Which of the following characteristics of atherosclerotic plaques is associated with the GREATEST risk of rupture?
- Abundant smooth muscle cells
- Minimal extracellular lipid
- Rare foam cells
- Scattered inflammatory cells
- Thin fibrous cap
ANSWER
CASE NUMBER 28
[ImageScope] [WebScope]
Clinical History: A 27-year-old woman was brought to the Emergency Department following a loss of consciousness. On presentation, her BP was 94/57 mmHg in her right arm and 89/54 mmHg in her left arm. Her heart rate was 106 beats per minute. O2 sat was 93% on RA. CV exam showed a tachycardic rate with regular rhythm. Lungs were clear to auscultation bilaterally. Neurological exam showed no focal findings. She was sent for a CT of her chest with contrast to evaluate for pulmonary embolism. While she was undergoing a chest CT, she became hypotensive and unresponsive and died.
Image Gallery:
(Summary of Gross Findings - click here)
At the top left of the image, there is a focus of cardiac muscle. An aortic dissection begins just distal to this point (at the aortic root) and continues through the ascending, descending and abdominal aorta as shown in the next two images. There is minimal atherosclerosis.
|
(Summary of Radiologic Findings - click here)
A chest CT shows pericardial effusion (asterisk) and abdominal aortic dissection (arrowhead).
|
|
(Summary of Microscopic Findings - click here)
There is a blood-filled tear between the inner 2/3 and outer 1/3 of the media. Note necrosis and deposition of fibrin along the margins of the defect. The remainder of the media contains the changes of "cystic medial necrosis.
|
(Review Normal Histology - click here)
Norm No. 9 Aorta
[ImageScope] [WebScope]
The aorta is a large elastic artery. The luminal surface is lined by flat endothelial cells. This is called the “intima”. Adjacent to the intima is the internal elastic lamina. This is composed of elastin and has a corrugated appearance on histological section. Adjacent to the internal elastic lamina is the tunica media which is composed of smooth muscle. Finally, the outermost layer is the adventitia which is composed of connective tissue.
|
28-1. Based on the findings thus far, what is the differential diagnosis?
ANSWER
28-2. Which of the following is MOST COMMONLY associated with this diagnosis?
- Antithrombin III deficiency
- Atherosclerosis
- Hypertension
- Syphilis
- Vitamin C deficiency
ANSWER
28-3. Which of the following should be suspected in this patient?
- Bacterial sepsis
- Cardiogenic shock
- Connective tissue abnormalities
- Fat embolism
- Heroin use
ANSWER
CASE NUMBER 158
[ImageScope] [WebScope]
Clinical History: A 63-year-old man presented to the emergency department with a two-day history of severe chest pain and dyspnea. Past medical history was relevant for a 5-year history of congestive heart failure and progressive weakness. While he was in the emergency department, he collapsed and died. Gross and microscopic images from the autopsy are provided.
Image Gallery:
(Summary of Gross and Lab Findings - click here)
The lung was dark red and heavy, and a large amount of hemorrhagic frothy fluid exuded freely from the cut surface. In the main pulmonary artery there was a large red firm clot adherent to the vascular wall. Many small blood clots were present in the vessels of the upper and lower lobes. Associated with these were many wedge-shaped, dark red, firmer areas in the lung parenchyma.
|
(Summary of Microscopic Findings - click here)
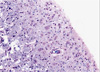
There are two sections on the slide. On one section there are organizing thrombi in the pulmonary arteries. On the other section there is a large hemorrhagic area in which some alveolar septa are pink, smudgy, and necrotic. In other portions of the lung the septa are thickened with fibrosis.
|
(Review Normal Histology - click here)
Norm No. 24 Lung
[ImageScope] [WebScope]
The primary function of the lung is gas exchange. Therefore, alveoli have thin walls lined by thin flat pneumocytes and endothelial cells. There is no thickening or fibrosis of the interstitium. The bronchioli are lined with basally oriented ciliated columnar epithelium. The bronchi are lined by similar epithelium. There are mucous glands within the submucosa. The bronchial smooth muscle is not hypertrophied. The pulmonary vessels are patent with no evidence of intimal thickening or muscular hyperplasia.
|
158-1. What is the differential diagnosis?
ANSWER
158-2. What do the firm, red, wedge-shaped areas of the lung represent?
- Angiosarcoma
- Hemorrhage
- Infarcts
- Metastatic disease
- Thrombosis
ANSWER
158-3. In cases of deep venous thrombosis with embolism, which vessels are MOST OFTEN occluded?
- Bronchial arteries
- Bronchial veins
- Inferior vena cava
- Pulmonary arteries
- Pulmonary veins
- Superior vena cava
ANSWER
158-3. Pulmonary emboli are more common than pulmonary infarcts. Which of the following explains this observation?
- Coagulation is slower in oxygenated tissue
- Lung tissue has increased numbers of mitochondria
- Lungs have a dual arterial supply
- Oxygenation can occur across the bronchial wall
- Venous drainage is accelerated in lung tissue
ANSWER
CASE NUMBER 370 - slide courtesy of UMich
[ImageScope] [WebScope]
Clinical History: A 67-year-old woman with a long history of hypertension and a remote myocardial infarction presented to the emergency department with a two-hour history of left-sided weakness. She reported that she had a “fluttering” sensation in her chest and that her cardiologist had recommended treatment for atrial fibrillation which she had refused. While in the emergency department, she developed left-sided hemiparesis. She was admitted to the hospital for observation; however, her condition worsened and she went into a coma. She died 17 days after admission.
Image Gallery:
(Summary of Gross Findings - click here)
There is a recent infarct in the right middle cerebral artery territory which involved the primary motor cortex as well as the lenticulostriate arteries serving the putamen, caudate, and internal capsule.
|
(Summary of Microscopic Findings - click here)
This is a luxol stain, which stains cell bodies (most abundant in the cortex) light pink whereas myelin (most abundant in the white matter) is dark blue. There is an area of liquefactive necrosis in the infarcted cerebral cortex. The myelin in this area stains pale due to surrounding edema fluid. The blood vessels are congested and there is some extravasated blood.
|
(Review Normal Histology - click here)
Cerebrum
Slide 76 (cerebrum, luxol blue/cresyl violet) [WebScope] [ImageScope]
Slide 76b (toluidine blue & eosin) [WebScope] [ImageScope]
The cerebral cortex is loosely stratified into layers containing scattered nuclei of both neurons and glial cells. Examine the layered organization of the cerebral cortex using slide 76 stained with luxol blue/cresyl violet [ORIENTATION] (which stains white matter tracts and cell bodies) or toluidine blue and eosin [ORIENTATION] (TB&E, toluidine blue stains the nuclei and RER of cells whereas eosin stains membranes and axon tracts). Typically one or more sulci (infoldings) will extend inward from one edge of the section. Examine the gray matter on each side of the sulcus using first low and then high power. Neurons of the cerebral cortex are of varying shapes and sizes, but the most obvious are pyramidal cells. As the name implies, the cell body is shaped somewhat like a pyramid, with a large, branching dendrite extending from the apex of the pyramid toward the cortical surface, and with an axon extending downward from the base of the pyramid. In addition to pyramidal cells, other nuclei seen in these sections may belong to other neurons or to glial cells also present in the cortex. You may be able to see subtle differences in the distribution of cell types in rather loosely demarcated layers. There are 6 classically recognized layers of the cortex:
- Outer plexiform (molecular) layer: sparse neurons and glia
- Outer granular layer: small pyramidal and stellate neurons
- Outer pyramidal layer: moderate sized pyramidal neurons (should be able to see these in either luxol blue [example] or TB&E-stained [example] sections)
- Inner granular layer: densely packed stellate neurons (usually the numerous processes aren’t visible, but there are lots of nuclei reflecting the cell density)
- Ganglionic or inner pyramidal layer: large pyramidal neurons (should be able to see these in either luxol blue [example] or TB&E-stained [example] sections)
- Multiform cell layer: mixture of small pyramidal and stellate neurons
Pyramidal cells in layers III and V tend to be larger because their axons contribute to efferent projections that extend to other regions of the CNS –pyramidal neurons in layer V of motor cortices send projections all the way down to motor neurons in the spinal cord!
Deep to the gray matter of the cerebral cortex is the white matter that conveys myelinated fibers between different parts of the cortex and other regions of the CNS. Be sure you identify the white matter in both luxol blue [example] and TB&E-stained [example] sections, as it will appear differently in these two stains. Review the organization of gray and white matter in cerebral cortex vs. spinal cord.
|
370-1. What is the differential diagnosis?
ANSWER
370-2. Which of the following is the most likely cause of the morphologic findings?
- Direct parenchymal injury
- Hypotension
- Infectious vasculitis
- Thromboembolism
- Traumatic vascular injury
ANSWER
370-3. What is the most likely etiology of her condition?
- Atrial fibrillation
- Deep venous thrombosis
- Disseminated intravascular coagulation (DIC)
- Factor V mutation
- Protein C deficiency
ANSWER
370-4. The enlarged, foamy cells seen in the high power histologic image are most likely:
- Lymphocytes
- Macrophages
- Neurons
- Neutrophils
- Astrocytes
ANSWER
CASE NUMBER 514
(no virtual slides for this case)
Clinical History: A 28-year-old woman presents to the Emergency Department with an acute onset of severe dyspnea after disembarking from a trans-Atlantic flight. She reports left-sided chest pain on inspiration. She has no significant medical history, but states that she takes oral contraceptive pills. Physical exam shows 20 breaths per minute and a heart rate of 125 bpm. Her left calf is swollen and warm. A duplex ultrasound demonstrates a deep venous thrombosis. Laboratory analysis reveals a positive activated protein C resistance test; remaining studies are noncontributory.
Image Gallery:
514-1. Which of the following is the most likely etiology for her condition?
- Antiphospholipid antibody syndrome
- Factor V Leiden mutation
- Glucose-6-phosphate dehydrogenase deficiency
- Hyperhomocystenemia
- von Willebrand disease
ANSWER
514-2. Which of the following is true about this disease?
- Homozygotes have a 50-fold increase in relative risk of venous thrombosis
- Inheritance is typically autosomal recessive
- It is associated with increased prothrombin levels
- Partial thromboplastin time is typically prolonged
- There is an increased incidence in patients with systemic lupus erythematosus
ANSWER
514-3. Which of the following is the pathophysiology of this disease?
- Autoantibodies cause platelet aggregation
- Factor V is resistant to cleavage
- Prothrombin is resistant to cleavage
- Thioester linkages form between homocysteine metabolites and proteins
- Ultra large von Willebrand multimers are found in the serum
ANSWER
514-4. Genetic analysis would most likely show which of the following?
- A chromosomal translocation
- A missense mutation
- A nonsense mutation
- A partial deletion of chromosome 12
- Ring chromosomes
ANSWER
Review Items
THROMBOSIS, HEMOSTASIS, EDEMA, and SHOCK - Key Vocabulary Terms
HEMODYNAMICS AND ARTERIOSCLEROSIS - Key Vocabulary Terms
GOALS and LEARNING OBJECTIVES
Goal 1: Hemodynamics and Shock
Apply knowledge of the biochemical and cellular physiology to discuss the pathogenic mechanisms resulting in alterations in hemodynamics and shock. Describe the resulting pathology at the cellular, tissue and organism level and describe clinical manifestations associated with these pathologic changes.
- Objective 1: Edema
Describe the pathophysiologic categories of edema and compare and contrast, with examples, how edema can be produced as a result of changes in hydrostatic pressure or plasma oncotic pressure.
- Objective 2: Hyperemia and Hemorrhage
Explain the clinical, morphological, and physiological significance of hyperemia, congestion and hemorrhage.
- Objective 3: Shock
Classify different types of shock according to etiology and compare and contrast the pathogenesis of these different types.
Goal 2: Clotting and Disruption of Blood Flow
Apply knowledge of the biochemical and cellular physiology to discuss pathogenetic mechanisms that result in alterations in blood clotting or other disruptions to blood flow. Describe the resulting pathology at the cellular, tissue and organism level and the clinical manifestations associated with these pathologic changes.
- Objective 1: Blood Clotting
Discuss the vascular, cellular and humoral events involved in blood clotting, and provide examples of genetic or acquired factors that can lead to either excess clotting or bleeding.
- Objective 2: Thrombosis and Thromboembolism
Compare and contrast thrombosis in situ and thromboembolism with respect to sites of involvement, risk factors, and attendant pathologic and clinical consequences.
- Objective 3: Embolism
Compare and contrast the etiology and clinical consequences of different types of embolism
Goal 3: Platelets
Apply knowledge of platelet structure and function to discuss qualitative and quantitative disorders leading to abnormal bleeding.
- Objective 1: Platelets in Hemostasis
Summarize the role played by platelets in hemostasis, including platelet adhesion, activation, and aggregation.
- Objective 2: Thrombocytopenia
Identify the examples of each of the following pathogenetic categories of thrombocytopenia: decreased production, decreased platelet survival, sequestration, dilutional effect.
- Objective 3: Thrombocytopenic Syndromes
Compare and contrast the following thrombocytopenia syndromes: immune thrombocytopenic purpura, drug-induced thrombocytopenia, heparin-induced thrombocytopenia.
- Objective 4: Thrombocytopenic Purpura
Compare and contrast thrombotic thromobocytopenic purpura with hemolytic uremic syndrome.
Goal 4: Hemostasis
Apply knowledge of normal hemostasis, interaction of platelets, and procoagulant and anticoagulant factors to describe qualitative and quantitative disorders leading to abnormal bleeding and thrombosis.
- Objective 1: Types of Hemorrhage
Distinguish among the following manifestations of hemorrhage: hematoma, petechiae, purpura, and ecchymoses.
- Objective 2: Stages of Hemostasis
Compare and contrast the following stages of hemostasis: vasoconstriction, primary hemostasis, secondary hemostasis, and antithrombotic counterregulation.
- Objective 3: Secondary Hemostasis
Outline the process of secondary hemostasis, in terms of intrinsic pathway, extrinsic pathway, common pathway, fibrin formation, and fibrinolysis.
- Objective 4: Proteases and the Coagulation Cascade
Describe how particular proteins that regulate the proteases to activate the clotting cascade either promote or inhibit coagulation.
- Objective 5: Mechanisms of Hypercoagulability
Compare and contrast the roles of endothelial injury, stasis, and alterations in the regulation of blood clotting in the development of the hypercoagulable state.
- Objective 6: Risk Factors for Thrombophilia
Give examples and discuss the pathophysiology of inherited versus acquired conditions that increase the risk of thrombophilia.
- Objective 7: Disseminated Intravascular Coagulopathy
Discuss disseminated intravascular coagulopathy (DIC) in terms of etiologies, pathogenesis, clinical presentation, and course.
- Objective 8: Inherited Hemophilia
Discuss the pathogenesis and clinical and laboratory manifestations of hemophilia A and explain how it differs from hemophilia B.
- Objective 9: von Willebrand Disease
Compare and contrast types I, II, and III von Willebrand disease and explain the quantitative or qualitative abnormalities and the laboratory features observed in each type.
- Objective 10: Heparin-Induced Thrombocytopenia
Explain the mechanism of heparin-induced thrombocytopenia/thrombosis and describe its clinical presentation and approach to therapy.
Goal 5: Mechanisms of Atherosclerosis
Apply knowledge of immunologic principles, inflammation, and tissue repair to explain atherosclerosis and its complications.
- Objective 1: Factors Contributing to Endothelial Injury
Explain how environmental factors (including elevated cholesterol and LDL complexes, infection, and smoking) can contribute to endothelial cell injury.
- Objective 2: Feedback in Endothelial Damage
Describe the positive feedback loop in which damaged endothelial cells cause further endothelial damage.
- Objective 3: Atherosclerosis Plaque Rupture
Predict the local and distant consequences that are likely to follow rupture of an atherosclerotic plaque and the resultant clinical presentation.
- Objective 4: Vascular Aneurysm
Describe the morphologic changes in atherosclerosis and discuss how atrophic changes in the vessel wall may result in aneurysm formation.
Goal 6: Vascular Damage and Thrombosis
Apply knowledge of the cellular response to injury and basic hemodynamic principles to explain how defective or excessive inflammatory and reparative processes damage blood vessels and how this damage results in thrombus formation.
- Objective 1: Thrombus Formation
Discuss the steps in thrombus formation and its predisposing factors.
- Objective 2: Aortic Aneurysm and Dissection
Compare and contrast aortic aneurysms and aortic dissections in terms of their predisposing factors, the sites of involvement, and patient populations likely to be affected.
- Objective 3: Abdominal Aortic Aneurysm
Describe the clinical consequences of an abdominal aortic aneurysm.
|
|
|