Case assignments by lab group and class day:
| |
TUESDAY |
THURSDAY |
Labs 1, 2, & 3 |
|
|
Labs 4 & 5 |
|
|
CASE NUMBER 190
[ImageScope] [WebScope]
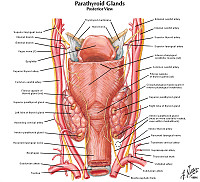
Clinical History: A 27-year-old woman presented to her primary care physician with a five-month history of episodic palpitations, dizziness and diaphoresis. In addition, she has had frequent headaches that do not improve with over-the-counter medication. Her family history is significant for an older brother who was diagnosed with a medullary carcinoma of the thyroid. On physical exam, her blood pressure is 230/125. Laboratory tests are significant for a serum calcium of 14 mg/dL.
An abdominal ultrasound showed a left-sided suprarenal mass. Subsequently, an MRI was performed.
190-1. What is the differential diagnosis?
ANSWER
Image Gallery:
(Summary of Imaging Findings)
This is an coronal T2-weighted (fluid is bright, fat is intermediate to bright) MRI that shows a hyperintense mass superior to the left kidney. Pheochromocytomas are often markedly hyperintense on T2 (this is referred to as the “lightbulb sign” but it is neither specific nor sensitive. Pheochromocytomas are often heterogeneous and show intermediate to high T2 signal intensity.
|
(Summary of Gross Findings)
There is an approximately 5 cm gray-tan mass that composes the majority of the specimen. The residual adrenal gland can be seen at the right of the image and as thin residual cortex stretching superiorly and inferiorly over the mass. library.med.utah.edu
|
(Summary of Microscopic Findings)
The section shows a portion of normal adrenal gland in the inferior portion of the slide with a cellular neoplasm arising on the superior aspect. The neoplasm consists of cells that resemble the normal adrenal medulla growing in nests separated by prominent blood vessels.
|
(Review Adrenal Histology)
Norm No. 11 Adrenal gland
[ImageScope] [WebScope]
Adrenal tissue is composed of a central medulla and outer cortex. The medulla contains large polygonal neuroendocrine cells. The cortex contains cells with foamy cytoplasm. There is no evidence of hemorrhage or necrosis.
|
|
190-2. Which of the following presurgical laboratory tests would confirm the diagnosis?
- Serum gastrin
- Serum prolactin
- Serum uric acid
- Urine albumin
- Urine free catecholamines
ANSWER
190-3. Which of the following syndromes is most likely in this patient?
- Multiple endocrine neoplasia type 1
- Multiple endocrine neoplasia type 2A
- Multiple endocrine neoplasia type 2B
- Neurofibromatosis type 1
- Von-Hippel Lindau syndrome
ANSWER
190-4. Molecular analysis of this tumor would most likely show mutation in which of the following genes?
- BRAF
- GNAS
- MEN1
- RAS
- RET
ANSWER
190-5. What is the so-called “rule of 10s” in regard to this tumor?
ANSWER
CASE NUMBER 264
[ImageScope] [WebScope]
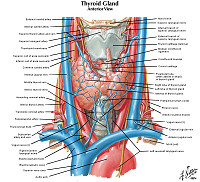
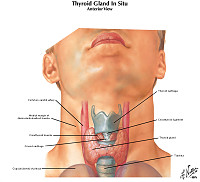
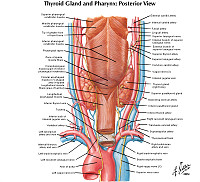
Clinical History: A 38-year-old Caucasian woman presented to her primary care physician with a three-month history of a neck mass and increasing dysphagia. She stated that over the previous 6 months she had been feeling fatigued and had little energy. Physical exam revealed a diffusely enlarged, symmetrical thyroid gland. Laboratory tests revealed thyroid stimulating hormone of 190 uIU/mL (0.34-5.66) and free thyroxine of 0.2 ng/dL (0.52-1.21). A total thyroidectomy is performed.
264-1. What is the differential diagnosis?
ANSWER
Image Gallery:
(Summary of Gross Findings)
At the time of surgery the entire thyroid was enlarged, with an estimated weight of 60 grams. The tissue was pale and lobulated. A subtotal thyroidectomy was performed. The excised tissue weighed 30 grams.
|
(Summary of Microscopic Findings)
The architecture of the gland is destroyed. A few acini are present. These vary in size. There is abundant lymphoid tissue in which are germinal centers. There are collections of rather large cells which do not form acini.
|
(Review Thyroid Histology)
Norm No. 5 Thyroid
[ImageScope] [WebScope]
Thyroid tissue consists of variably-sized, colloid-filled follicles. The colloid is eosinophilic and homogeneous. The glandular thyroid cells are cuboidal. The capsule is intact.
|
|
264-2. Which of the following is most accurate regarding this disease?
- Granulomatous inflammation is a characteristic feature
- Men are affected more commonly than women
- Most patients present with symptoms of hyperthyroidism
- Pathogenesis relates to autoantibodies against TSH receptor
- Patients are at increased risk for B cell non-Hodgkin lymphoma
ANSWER
264-3. Which of the following are typical clinical findings in this disease?
- Audible bruit over the thyroid gland
- Exophthamos
- Diffuse, symmetric enlargement of the thyroid gland
- Hard and fixed thyroid mass
- Pretibial myxedema
ANSWER
264-4. Antibodies against which of the following are most commonly seen in this disease?
- Calcitonin
- T3
- Thyroid peroxidase (TPO)
- Thyrotroph cells
- TSH receptor
ANSWER
CASE NUMBER 430
[ImageScope] [WebScope]
Clinical History: A 33-year-old woman presented to her primary care physician after she noticed a nodule in her neck, just to the left of midline, two months earlier. An ultrasound showed an irregularly shaped, solitary mass with small punctate areas suggestive of calcifications. Laboratory studies showed no abnormalities in thyroid function. She underwent a partial thyroidectomy. Gross and microscopic images are provided.
430-1. What is the differential diagnosis?
ANSWER
Image Gallery:
(Summary of Gross Findings)
Sectioning through a lobe of excised thyroid gland reveals a papillary carcinoma. This neoplasm can be multifocal, as seen here, because of the propensity of this neoplasm to invade lymphatics within thyroid, and lymph node metastases are common. The larger mass shown here is cystic and contains papillary excresences.
|
(Summary of Microscopic Findings)
The tumor is composed of papillae covered by closely packed cells with bland, sometimes optically-clear ("Orphan-Annie eye") nuclei. Nuclear grooves are also present. A few round purplish calcifications, termed psammoma bodies, are also seen.
|
(Review Thyroid Histology)
Norm No. 5 Thyroid
[ImageScope] [WebScope]
Thyroid tissue consists of variably-sized, colloid-filled follicles. The colloid is eosinophilic and homogeneous. The glandular thyroid cells are cuboidal. The capsule is intact.
|
|
430-2. Which of the following is a characteristic feature of this tumor?
- Amyloid deposition
- Capsular and vascular invasion
- Enlarged, pleomorphic giant cells
- Nuclear grooves and pseudoinclusions
- Prominent lymphocytic infiltrate
ANSWER
430-3. Which of the following is most accurate regarding this tumor?
- Exposure to ionizing radiation is a significant risk factor
- Hashimoto thyroiditis is a precursor lesion
- Isolated cervical lymph node metastasis is associated with <25% 5-year survival
- PAX8-PPARG fusions are seen in up to one-half of cases
- This tumor is a component of MEN type 2A
ANSWER
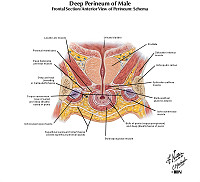
CASE NUMBER 202
[ImageScope] [WebScope]
Clinical History: A 74-year-old man presented to his primary care physician with a one-year history of hesitancy, intermittency, nocturia and increasing difficulty in urination. Rectal examination revealed an enlarged, nodular firm prostate. A week after his visit, he experienced a myocardial infarction and died. Autopsy findings revealed the gross and microscopic findings below.
202-1. What is the differential diagnosis?
ANSWER
Image Gallery:
(Summary of Gross Findings)
The prostate was large, nodular, and 120 grams in weight. The capsule was tense, and many gray-white firm nodules bulged out of the cut surface. These nodules varied from 3 mm to 1 cm. The larger ones were present in the lateral lobes and compressed the urethra.
|
(Summary of Microscopic Findings)
Two types of nodules can be distinguished. One is composed essentially of fibro-muscular elements - stromal hyperplasia. The other is composed predominantly of epithelial glands. The size of the glands varies remarkably, and cystic dilatation of some is present. There are two types of cells forming the glands. The luminal cells are tall columnar cells with basal nuclei and apocrine secretory activity in the cytoplasm. The basal cell layer is composed of cuboidal or flattened epithelium. These glandular nodules are well demarcated by the encircling fibro-muscular stroma.
|
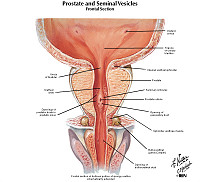
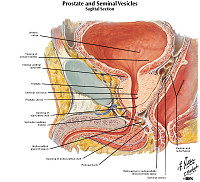
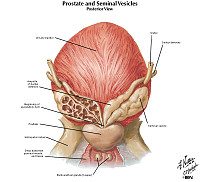
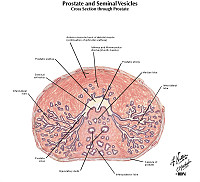
(Review Prostate Histology)
Norm No. 1 Prostate
[ImageScope] [WebScope]
The prostate gland is composed of multiple glandular spaces lines by a basal layer of cuboidal epithelium covered by columnar secretory cells with frequent papillary projections into the gland lumen. The cells are uniform in size and shape. The nuclei are not crowded. They do not have nucleoli that are visible. Glands are separated by fibrovascular stroma.
|
|
202-2. Which of the following factors contributes most significantly to the development of this condition?
- Arylamine exposure
- Bladder stones
- Cigarette smoking
- Circulating androgens
- Hypertension
ANSWER
202-3. Patients with this condition are at significantly increased risk for which of the following?
- Adenocarcinoma of the prostate
- Condyloma acuminatum
- Priapism
- Pyelonephritis
- Spermatocytic seminoma
ANSWER
CASE NUMBER 5
[ImageScope] [WebScope]
Clinical History: A 77-year-old man went to his primary care physician for an annual checkup. Digital rectal exam revealed a firm nodule at the base of the prostate gland. Serum PSA was measured at 7.0 ng/mL (normal < 4.0 ng/mL). Needle biopsies were performed and the patient subsequently underwent a total prostatectomy. Gross and microscopic images are provided.
5-1. What is the differential diagnosis?
ANSWER
Image Gallery:
(Summary of Gross Findings)
The prostate was quite large and firm with multiple rubbery nodules measuring 2 mm to 6 mm in diameter. Some of the nodules contain yellowish flecks. The seminal vesicles were firm bilaterally.
|
(Summary of Microscopic Findings)
There are a number of glands shown in varied patterns. In some cases the epithelial cells are found in non-glandular masses. The epithelial cells are cuboidal or polygonal with central, round, deeply pigmented nuclei. Few, if any, mitotic figures can be seen. The presence of perineural and perivascular invasion is clearly in evidence. This is a useful diagnostic characteristic of adenocarcinoma of the prostate.
|
(Review Prostate Histology)
Norm No. 1 Prostate
[ImageScope] [WebScope]
The prostate gland is composed of multiple glandular spaces lines by a basal layer of cuboidal epithelium covered by columnar secretory cells with frequent papillary projections into the gland lumen. The cells are uniform in size and shape. The nuclei are not crowded. They do not have nucleoli that are visible. Glands are separated by fibrovascular stroma.
|
|
5-2. Which of the following features is most characteristic of this lesion?
- Absence of a basal cell layer
- Extensive calcification
- Marked nuclear pleomorphism
- “Salt and pepper” chromatin
- Squamous pearls
ANSWER
5-3. The Gleason grading system is based on which of the following features?
- Degree of gland formation
- Nuclear pleomorphism
- Number of mitotic figures
- Perineural invasion
- Presence of necrosis
ANSWER
5-4. Following his prostatectomy, the patient’s PSA level dropped to essentially zero. However, two years later, his serum PSA was again elevated. Which of the following is most accurate concerning serum PSA?
- Current treatment recommendations include routine screening of PSA levels for all men over 65.
- Even mildly elevated levels of PSA are highly suggestive of malignancy.
- Following prostatectomy, serum PSA is a good marker of residual, recurrent or metastatic disease.
- Serum PSA is a good screening test for undiagnosed prostate cancer.
- Serum PSA is rarely elevated in benign conditions.
ANSWER
CASE NUMBER 34
[ImageScope] [WebScope]
Clinical History: A 35-year-old man presented to his primary care physician with non-specific testicular discomfort and stated that he has noticed that his right testicle felt larger than his left testicle. Physical exam revealed enlargement of the right testis, which did not transilluminate. The patient underwent a right orchiectomy. Gross and microscopic images are provided.
34-1. What is the differential diagnosis?
ANSWER
Image Gallery:
(Summary of Gross Findings)
The orchiectomy specimen has been opened to demonstate the soft fleshy tumor which has replaced the normal testis. The spermatic cord is attached.
|
(Summary of Microscopic Findings)
Note the characteristic arrangement of cells in small groups outlined by delicate fibrous stroma. The cells are relatively uniform with distinct borders. The cytoplasm is clear and sometimes almost foamy. The cells are polygonal with large, round, central nuclei and prominent nucleoli. In many sections a fragment of atrophic and fibrotic testis may be seen adjacent to the tumor.
|
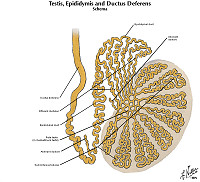
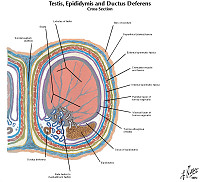
(Review Testis Histology)
Norm No. 22 Testis
[ImageScope] [WebScope]
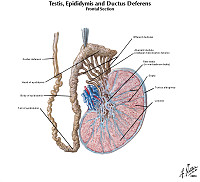
The testis is the male gland responsible for sperm production. There is a fibrous capsule and multiple glands separated by a loose stoma. Within the glands there are mature and immature sperm. Within the stroma there are a few large Leydig cells which are responsible for testosterone production.
|
|
34-2. Markedly elevated serum HCG levels in this patient would suggest which of the following?
- AFP will also be elevated
- More than one germ layer is present
- Radiation is the best therapy
- Schiller-Duval bodies will be seen microscopically
- This is a mixed tumor
ANSWER
34-3. Which of the following tumors is most sensitive to radiation therapy?
- Choriocarcinoma
- Embryonal carcinoma
- Sertoli cell tumor
- Seminoma
- Yolk sac tumor
ANSWER
ENDOCRINE Review Items
Key Vocabulary Terms (click here to search any additional terms on Stedman's Online Medical Dictionary)
| 17-hydroxycorticosteroids |
glycosyation (glycation) |
parathyroid hormone related protein |
| 17-ketosteroids |
goiter |
parathyroid hyperplasia |
| acromegaly |
goiter, diffuse nontoxic (simple) |
pheochromocytoma |
| acute adrenal cortical insufficiency |
goiter, multinodular |
pinealomas |
| Addison disease |
goiter, sporadic |
plasma renin activity |
| adrenal cortical adenomas |
goitrogen |
plasma renin concentration |
| adrenal cortical carcinomas |
Graves disease |
polydipsia/polyphagia/polyuria |
| adrenocorticotropin (ACTH) |
growth hormone (GH) |
primary aldosteronism (Conn syndrome) |
| aldosterone |
growth hormone releasing hormone |
primary diabetes |
| aldosteronism, primary (Conn syndrome) |
hypercalcemia of malignancy |
pseudohypoparathyroidism |
| angiotensin |
hyperadrenalism |
radioactive iodine uptake (RAIU) |
| angiotensin converting enzyme |
hyperadrenocorticism |
radioimmunoassay |
| angiotensinogen |
hypercalcemia |
renin |
| bronze diabetes |
hyperinsulinism |
secondary aldosteronism |
| catecholamine |
hyperosmolar nonketotic coma |
secondary diabetes |
| congenital adrenal hyperplasia |
hyperparathyroidism |
Sheehan syndrome |
| congenital adrenal hypoplasia |
hyperparathyroidism, primary |
Sipple syndrome |
| corticotropin-releasing hormone (CRH) |
hyperparathyroidism, secondary |
somatomedin (IGF) |
| cortisol |
hyperparathyroidism, tertiary |
somatostatin |
| cortisol binding globulin (CBG) |
hyperpituitarism |
steroid hydroxylase enzymes |
| craniopharyngioma |
hyperthyroidism |
thyroglobulin |
| cretinism |
hypocalcemia |
thyroid adenomas |
| Cushing disease |
hypoparathyroidism |
thyroid carcinomas |
| Cushing syndrome |
hypopituitarism |
thyroid stimulating hormone (TSH) |
| dexamethasone suppression test |
hypothyroidism |
thyrotoxicosis |
| diabetes insipidus |
impaired glucose tolerance |
thyroiditis, Hashimoto's |
| diabetes mellitus |
inappropriate ADH |
thyroiditis, infectious |
| diabetic ketoacidosis |
insulin resistance |
thyroiditis, Riedel's |
| ectopic ACTH |
ionized calcium |
thyroiditis, subacute (granulomatous) |
| empty sella syndrome |
endocrine neoplasia (MEN) syndrome |
thyroiditis, subacute lymphocytic, |
| endemic goiter |
myxedema |
thyrotropin releasing hormone (TRH) |
| epinephrine |
neuroblastoma |
thyroxine (T4) |
| euthyroidism |
norepinephrine |
thyroxine binding globulin (TBG) |
| free thyroxine index (FTI) |
parathyroid adenoma |
triiodothyronine (T3) |
| ganglioneuroma |
parathyroid carcinoma |
vanillylmandelic acid (VMA) |
| gestational diabetes |
parathyroid hormone (PTH) |
Waterhouse-Friderichsen syndrome |
| gigantism |
|
|
ENDOCRINE PATHOLOGY LEARNING OBJECTIVES
Goal 1: Hyper- and Hypopituitarism
Apply knowledge of pituitary physiology to describe the pathophysiology and clincopathologic features of disorders associated with hyperpituitarism and hypopituitarism.
Objective 1.1: Anterior Pituitary
List several causes for destruction of the anterior pituitary and the clinicopathologic features associated with each.
Objective 1.2: Sheehan Syndrome
Define Sheehan syndrome and the clinicopathologic features associated with it.
Goal 2: Hyper- and Hypothyroidism
Apply knowledge of thyroid physiology to explain the pathophysiology and clincopathologic features, including laboratory findings, of disorders associated with hyperthyroidism and hypothyroidism.
Objective 2.1: Causes of Hyper- and Hypothyroidism
Compare and contrast the causes of hyperthyroidism and hypothyroidism.
Goal 3: Autoimmune Thyroiditis
Apply knowledge of immune system dysregulation to summarize immune-related disorders of the thyroid.
Objective 3.1: Graves Disease, Hashimoto and Subacute Thyroiditis
Compare and contrast the pathophysiology and clinicopathologic features, including laboratory findings, of Graves disease, Hashimoto thyroiditis, and subacute lymphocytic thyroiditis.
Objective 3.2: Granulomatous Thyroiditis
Compare and contrast immune-mediated thyroid disease with subacute granulomatous thyroiditis (DeQuervain thyroiditis).
Goal 4: Hyper- and Hypoadrenalism
Apply knowledge of adrenal physiology to describe the pathophysiology and clincopathologic features of disorders associated with adrenocortical hyperfunction (hyperadrenalism) and adrenocortical insufficiency.
Objective 4.1: Cushing Syndrome
Compare and contrast the causes and clinicopathologic features of hypercortisolism (Cushing syndrome) and the pathophysiologic basis distinguishing between these causes and the management of this disease.
Objective 4.2: Hyperaldosteronism
Compare and contrast the causes and clinicopathologic features of hyperaldosteronism.
Objective 4.3: Congential Adrenal Hyperplasia
Outline the clinicopathologic features of congenital adrenal hyperplasia.
Objective 4.4: Adrenocortial Insufficiency
Compare and contrast the causes of adrenocortical insufficiency, including the pathogenesis of primary acute and chronic adrenocortical insufficiency.
Goal 5: Endocrine Neoplasms
Apply knowledge of the molecular basis of neoplasia to explain the clinical presentation, biologic behavior, morphologic appearance, classification, diagnosis, prognosis, and targeted therapy of endocrine neoplasms.
Objective 5.1: Pituitary Adenoma
Explain the clinicopathologic features of pituitary adenomas and their associated clinical syndromes.
Objective 5.2: Thyroid Neoplasms
Compare and contrast the clinicopathologic features of follicular adenomas, follicular carcinoma, medullary thyroid carcinoma and papillary thyroid carcinoma.
Objective 5.3: Pheochromocytoma and Paraganglioma
Outline the clinicopathologic features of pheochromocytoma and compare and contrast the hereditary cancer syndromes associated with paragangliomas/ pheochromocytomas.
Objective 5.4: Multiple Endocrine Neoplasia (MEN) Syndromes
Compare and contrast the clinicopathologic features of MEN 1 with MEN 2 and 3.
Goal 6: Endocrine Pancreas
Apply knowledge of the structure and function of the endocrine pancreas and biochemical principles of carbohydrate metabolism to summarize the clinicopathologic features, diagnostic criteria and therapy of disorders resulting from excess or decreased production of insulin and other islet cell hormones.
Objective 6.1: Features of Diabetes Mellitus
Compare and contrast the clinicopathologic features of type 1 and type 2 diabetes.
Objective 6.2: Complications of Diabetes Mellitus
Outline the pathologic complications of diabetes mellitus.
MALE GENITAL SYSTEM Review Items
Key Vocabulary Terms (click here to search any additional terms on Stedman's Online Medical Dictionary)
MALE UROGENITAL PATHOLOGY LEARNING OBJECTIVES
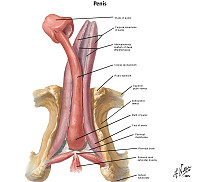
Goal 1: Penis
Apply knowledge of the embryology of the penis, infectious disease and principles of neoplasia to discuss the malformations and diseases of the penis.
Objective 1: Penile malformations
Compare and contrast hypospadias and epispadias in terms of clinical presentation and associated clinical findings.
Objective 2: Inflammatory Lesions of the Penis
Describe the inflammatory lesions of the penis in terms of their clinical setting, site of disease, organisms involved and the consequences of inflammation.
Objective 3: Neoplasms of the Penis
Describe the risk factors, epidemiology, pathologic findings and factors related to prognosis for neoplasms of the penis.
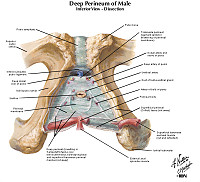
Goal 2: Nonneoplastic Disorders of the Prostate
Apply knowledge of the molecular and cellular origins of non- neoplastic disorders of the prostate, specifically prostatitis and nodular hyperplasia, to explain the epidemiology, clinicopathological features, natural history, and treatment strategy for these diseases.
Objective 1: Nodular Hyperplasia
Explain the molecular and hormonal origins of nodular hyperplasia, the area of the prostate affected, the natural history of the disease, various treatment strategies, and anticipated outcomes of treatment.
Objective 2: Prostatitis
Describe the pathophysiologic basis for inflammatory conditions affecting the prostate, including the organisms causing this condition.
Goal 3: Prostate Neoplasia
Apply knowledge of the molecular and cellular origins of prostate adenocarcinoma to summarize the epidemiology, clinicopathological features, natural history, and treatment strategies for this disease.
Objective 1: Prostate Adenocarcinoma
Outline the cellular phenotype of the typical adenocarcinoma cell and describe its molecular and immunohistochemical characteristics.
Objective 2: Histopathologic Criteria for Prostate Adenocarcinoma
Define the histopathological diagnostic criteria for the diagnosis and grading of adenocarcinoma.
Objective 3: Epidemiology of Prostate Adenocarcinoma
Explain the epidemiology of prostate cancer with respect to age, race, and family history.
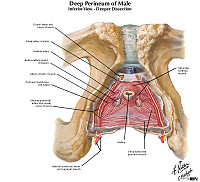
Goal 4: Nonneoplastic Disorders of the Testes
Apply knowledge of the molecular and cellular origins of non- neoplastic disorders of the testis to explain the epidemiology, clinicopathological features, natural history, and treatment strategy for these diseases.
Objective 1: Cryptorchism
Name the structure through which the testes descend during fetal development and what is brought with the testes in the descent and describe the complications of cryptorchidism.
Objective 2: Testicular Torsion
Describe the clinicopathologic features that occur in the testis due to torsion of the spermatic cord.
Objective 3: Orchitis
Discuss the inflammatory conditions affecting the testis and the clinicopathologic features associated with each.
Goal 5: Testicular Neoplasia
Apply knowledge of the molecular and cellular origins of the common types of testicular cancer to explain the epidemiology, clinicopathological features, natural history, and treatment strategies for this disease.
Objective 1: Diagnosis of the Testicular Mass
Discuss a differential diagnosis for a testicular mass.
Objective 2: Germ-Cell Tumors of the Testis
Describe the most important risk factors for development of a germ cell tumor of the testis and outline the clinicopathologic features for the different morphologic patterns seen.
Objective 3: Non-Germ Cell Tumors of the Testis
Describe the most important risk factors for development of a non-germ cell tumor of the testis and outline the clinicopathologic features for the different morphologic patterns seen.
Goal 6: Sexually Transmitted Diseases
Objective 1: Clinical Features of Sexually Transmitted Diseases
Discuss the common infections of the male and female genital tract including most common organisms, risk factors, clinical presentation and short- and long-term consequences of infection.
Objective 2: Pathologic Features of Sexually Transmitted Diseases
Compare and contrast the pathologic features of the various sexually transmitted diseases.
|