CASE NUMBER 502
[ImageScope] [WebScope]
Clinical History: A 73-year-old woman presented to her primary care physician with partial vision loss in her left eye. She additionally reported a two-week history of bitemporal headaches, fatigue and weight loss. Physical exam is significant for bilateral tenderness over the temporal areas. A biopsy of the temporal artery was performed.
Image Gallery:
(Summary of Physical Exam Findings)
Physical examination of the patient's temple shows a thickened, nodular, and tender segment of the superficial temporal artery.
|
(Summary of Microscopic Findings)
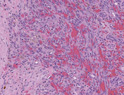
The superficial temporal artery exhibits significant thickening of the tunica intima, causing a reduction in lumenal diameter. There is extensive degradation of the internal elastic lamina as well as granulomatous inflammation consisting of an infiltrate of lymphocytes and macrophages within the tunica media. Numerous multinucleated giant cells are observed.
|
(Review of Blood Vessel Histology)
UMich Slide 42 (mesentery, H&E) WebScope ImageScope
UMich Slide 95M (mesentery, trichrome-elastin) WebScope ImageScope
These mesentery spreads contain numerous excellent examples small muscular arteries and their companion veins. Study the arteries first in slide #42 [example] , and/or #95 (trichrome) [example] . Note the thin intima, the distinct internal elastic lamina (IEL) and the media composed of circularly oriented smooth muscle cells. The media also contains some elastin and abundant “reticular” collagen, as well as specific proteoglycans. There is sometimes a condensation of elastic fibers in the outer portion of the media that may be an “external elastic lamina”, which varies from artery to artery. The adventitia is the dense, irregular connective tissue surrounding the media that varies in thickness. Remember that in blood vessels the components of the media are arranged circularly, while those of the adventitia are oriented longitudinally. In vessels where the media is too thick to be supported by simple diffusion, vasa vasorum (e.g. shown here in slide 95M) may also be observed in the adventitia.
The structure of the companion veins in slide #42 [example] and/or #95 (trichrome) [example] is less regular and may be difficult to understand at first, but still consists of the same basic layers as arteries with a tunica intima, media, and an adventitia, although the media is usually much less muscular and less organized compared to the companion artery. Conversely, the adventitia is usually thicker in veins and may often have some bundles of longitudinal smooth muscle [example] as well as vasa vasorum [example] . In some sections, you may be able to see a thin internal elastic lamina beneath the venular endothelium (particularly in slide #95M).
|
502-1. What is the differential diagnosis?
ANSWER
502-2. Which of the following is true regarding this disease?
- A negative arterial biopsy does not exclude this diagnosis
- Aortic dissection occurs in approximately 25% of patients
- Atypical B cells are the initiating stimulus
- There is a male predominance
- Vessels typically show continuous involvement
ANSWER
502-3. Which of the following is a rare but serious complication of this disease?
- Aortic dissection
- Atrophic gastritis
- Blindness
- Intracranial hemorrhage
- Renal failure
ANSWER
502-4. Which of the following vessels is most commonly affected by this disease?
- Coronary
- Pulmonary
- Renal
- Superior mesenteric
- Vertebral
ANSWER
CASE NUMBER 509
(no virtual slides for this case)
Clinical History: A 43-year-old woman presented to her primary care physician with a 3-month history of bilateral hand and wrist pain, stiffness and swelling. The stiffness is worse in the morning. A clinical image of her hands is provided.
Laboratory tests were positive for rheumatoid factor and anti-cyclic citrullinated peptide antibodies. Over the next 25 years, she had increasing pain and deformity of her hands and also experienced pain and swelling of her feet. A plain radiograph study is provided.
Image Gallery:
(Summary of Physical Exam Findings)
The hands are affected symmetrically. There is subluxation of the metacarpophalangeal (MCP) joints with prominent ulnar deviation. The proximal interphalangeal (PIP) joints are also affected. There is atrophy of the interosseous muscles and prominent ulnar deviation of the fingers.
|
(Summary of Radiologic Findings)
The imaging studies reflect the clinical findings. There is juxta-artiular osteopenia and subluxation of the metacarpophalangeal (MCP) joints with marginal erosions.
|
There is hypertrophy and hyperplasia of the synovial lining with a prominent mixed inflammatory infiltrate that includes lymphocytes and plasma cells. There is a lymphoid aggregate.
|
509-1. What is the differential diagnosis?
ANSWER
509-2. Which of the following is MOST CLOSELY associated with this disease?
- Deletion of 22q11
- Failure of B cell tolerance
- Hepatitis B infection
- HLA-DRB1
- Interferon alpha exposure
ANSWER
509-3. Which of the following antibodies are MOST LIKELY to be demonstrated in this patient?
- Anti-cyclic citrullinated peptides
- Anti-myeloperoxidase (MPO-ANCA)
- Anti-proteinase-3 (PR3-ANCA)
- Anti-smooth muscle
- Anti-transglutaminase (anti-eTg)
ANSWER
509-4. Which of the following is an important mediator and therapeutic target of this disease?
- Cryoglobulin
- Platelet-derived growth factor
- Toll-like receptor
- Transthyretin
- Tumor necrosis factor
ANSWER
CASE NUMBER 540
[ImageScope] [WebScope]
Clinical History: A 33-year-old man presents to a new primary care physician with a 6-month history of raised, reddish purple lesions on his trunk. He states that he has been having sex with men for more than ten years and that he has had unprotected sex multiple times. He says he went to a free clinic one month ago and a laboratory test was positive for HIV.
Image Gallery:
(Summary of Clinical Findings)
There are multiple discrete violaceous plaques with a somewhat linear appearance that are more or less aligned along Langer (ie. cleavage lines). They are more or less symmetric. They may appear pink to brown and may be confluent or discrete and have a macular, popular or nodular appearance.
|
(Summary of Microscopic Findings)
There is an atypical spindle cell proliferation that appears as an ill-defined nodule in the subcutaneous tissue. Discrete blood vessel formation is not seen; however, there are slit-like spaces with abundant extravasated red blood cells and hemosiderin-laden macrophages. There is associated fibrosis and lymphocytes. No significant pleomorphism is seen. There is no necrosis or brisk mitotic activity.
|
(Review Skin Histology)
Norm No. 15 Skin
[ImageScope] [WebScope]
Skin consists of keratinizing stratified squamous epithelium. The keratin layer is eosinophilic. Nuclei are not present. Beneath the keratin layer is a layer of flat epithelial cells with small pyknotic nuclei. Cells are regular and not crowded. These keratinocytes rest upon a layer of basal epithelium and a thin basement membrane. Beneath the epidermis is the dermis which consists of loose connective tissue. Within the dermis are sweat and sebaceous glands. Some slides contain hair follicles. There is no inflammation. The blood vessels are patent and do not contain thromboemboli.
|
540-1. What is the differential diagnosis?
ANSWER
540-2. Which of the following is most likely to be his CD4+ T cell count?
- <200 cells/uL
- Between 500 and 1000 cells/uL
- Between 1500 and 5000 cells/uL
- > 10,000 cells/uL
ANSWER
540-3. What are the three phases of HIV infection and how are they characterized?
ANSWER
540-4. He is prescribed with an antiretroviral therapy that includes a protease inhibitor. Which of the following is the mechanism of action of this drug?
- Enhances activation of CD8+ T cells
- Inactivates an HIV protease that attacks CD4+ T cells
- Increases ability of macrophages to lyse viral particles
- Lowers affinity of CCR5 and CXCR4 binding to gp120
- Prevents formation of mature proteins from gag and pol genes
ANSWER
540-5. A researcher is working on an experimental drug that kills all HIV-infected CD4+ T cells in a mouse model. He notices that even though all of these T cells are destroyed, he can still detect the presence of HIV in the mouse. Which of the following is the most likely reservoir for HIV in this system?
- B cells
- Basophils
- CD8+ T cells
- Eosinophils
- Macrophages
ANSWER
CASE NUMBER 19
[ImageScope] [WebScope]
Clinical History: A 51-year-old man with a long history of tuberculosis presented to his primary care physician with a 4-week history of bilateral ankle edema. Physical examination revealed an enlarged liver and urinalysis showed 2+ proteinuria. While he was being evaluated, he experienced a ventricular arrhythmia and died. Gross and microscopic images are provided.
Image Gallery:
(Summary of Gross Findings)
Both kidneys were large, each weighing 250 grams. This chronic renal disease may actually increase the size of the kidney. Pale deposits of amyloid are present in the cortex, most prominently at the upper center. The liver weighed 1900 grams and was firm with a waxy appearance. The heart (not shown) was also large, weighing 470 grams.
|
(Summary of Microscopic Findings)
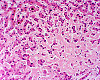
Kidney: The same type of hyaline pink material is present in the glomeruli, and is deposited between the endothelial cells and the basement membrane. In some places, it may be present in masses that encroach on the lumen of the capillary. The amyloid can also be recognized in the walls of some small arteries, and in a few places can be seen around the tubules in the interstitial tissue.
Liver: Most of the liver is replaced by homogenous, hyaline pink-staining amyloid which has been laid down between the sinusoids and the liver cells. This would stain with Congo red, or would be metachromatic if stained with crystal violet. The liver cords are replaced or compressed, and appear as widely separated thin cords of cuboidal cells. Bile plugs are present in the bile capillaries.
|
(Review of Normal Histology)
Kidney:
Norm No. 2 [ImageScope] [WebScope]
The kidney excretes soluble waste from the body and controls electrolyte balance. It consists of the cortex and the medulla. Within the outer cortex, glomeruli with delicate capillary loops are seen. The basement membrane is thin and without inflammation or thickening. Bowman’s capsule that surrounds the glomerulus is thin. The interstitium demonstrates no evidence of inflammation or fibrosis. In the areas between the glomeruli, tubules and arterioles are seen. The tubules are intact. The vessels exhibit no narrowing or wall thickening. The inner medulla of the kidney contains only tubules and blood vessels. Larger arteries and veins are located at the interface between cortex and medulla.
Liver:
Norm No. 3 [ImageScope] [WebScope]
The liver is the organ that metabolizes nutrients received from the digestive tract. These nutrients and processed by tissue hepatocytes which are large polygonal cells. The hepatocyes are separated by portal triads. The triads consist of an artery, a vein and a bile duct. The bile duct is lined by cuboidal epithelium. The artery has a muscular wall and a flat endothelial lining. The sinuses are well defined and contain a small amount of blood.
|
19-1. What is the differential diagnosis?
ANSWER
19-2.The development of this particular disease in this patient is MOST LIKELY due to deposition of which of the following?
- β-amyloid protein (Aβ)
- Amyloid light chain protein (AL)
- Amyloid-associated fibril protein (AA)
- β2-microglobulin
- Transthyretin
ANSWER
19-3. Which of the following stains is most commonly used to visualize the deposited substance?
- Congo red
- Oil Red O
- Periodic acid-Schiff
- Silver
- Warthin-Starry
ANSWER
19-4. Which of the following is the MOST COMMON cause of this disease?
- Familial Mediterranean fever
- Hemodialysis
- Plasma cell dyscrasia
- Rheumatoid arthritis
- Tuberculosis
ANSWER
CASE NUMBER 8
(no virtual slide for this case)
Clinical History: A 12-year-old boy with end-stage renal failure due to congenital ureteral obstruction received a living-donor renal transplant from his grandfather which failed eight years later due to noncompliance with immunosuppressive medications. At age 25, he received a second, deceased-donor renal transplant. His immunosuppressive regimen included tacrolimus (FK 506), azathioprine, and prednisone. His serum creatinine level fell during the first week post-transplant to almost normal levels, but then began to rise again, reaching a level of 5 mg/dL. A percutaneous renal biopsy was performed.
Image Gallery:
(Summary of Microscopic Findings)
The first two images, of H&E-stained sections, show renal tissue with a dense interstitial inflammatory infiltrate composed primarily of mononuclear inflammatory cells with occasional admixed neutrophils. A glomerulus is present in the first image and unremarkable in appearance, and tubules are largely spared by the inflammation, which seems to be centered on peritubular capillaries (located between the tubules and largely obscured by the inflammation). The final image, an immunofluorescent stain for the complement split product C4d, shows intense linear staining of peritubular capillaries. The staining pattern is due to a type II hypersensitivity reaction, which is typically linear (as opposed to type III, which is granular). The dark, non-staining areas between the capillaries are tubules.
|
(Review Normal Histology)
Norm No. 2
[ImageScope] [WebScope]
The kidney excretes soluble waste from the body and controls electrolyte balance. It consists of the cortex and the medulla. Within the outer cortex, glomeruli with delicate capillary loops are seen. The basement membrane is thin and without inflammation or thickening. Bowman’s capsule that surrounds the glomerulus is thin. The interstitium demonstrates no evidence of inflammation or fibrosis. In the areas between the glomeruli, tubules and arterioles are seen. The tubules are intact. The vessels exhibit no narrowing or wall thickening. The inner medulla of the kidney contains only tubules and blood vessels. Larger arteries and veins are located at the interface between cortex and medulla.
|
8-1. What is the differential diagnosis?
ANSWER
8-2. Which of the following would be the best test to confirm the diagnosis?
- Complete blood count with differential
- Evaluation of serum complement levels
- Examination of a peripheral blood smear
- Immunohistochemical stains for cytomegalovirus
- Screening for donor-specific antibodies
ANSWER
Clinical History (continued): Additional clinical information: Circulating antibodies against both class I and class II histocompatibility antigens were detected by serologic testing; one of the anti-class I antibodies was donor-specific.
8-3. Which of the following is the most likely cause of anti-HLA antibodies in this patient?
- Autoimmunity
- Immune reaction to drug-bound self proteins
- Immunization by cross-reacting gut flora
- Production of anti-graft antibody by neoplastic plasma cell clone
- Sensitization by previous allograft
ANSWER
8-4. This patient is at greatest risk for developing which of the following?
- Graft-versus-host disease
- Hyper-IgM syndrome
- IgA deficiency
- Non-Hodgkin lymphoma
- Wiskott-Aldrich syndrome
ANSWER
IMMUNOPATHOLOGY Review Items
Key Vocabulary Terms
LEARNING OBJECTIVES
Absolutely critical information you must know to practice medicine is in bold font.
Important information that will be needed for routine patient care is in regular font.
Information about less common diseases that you may encounter in clinical practice and that will probably appear on examinations is in italics
-
Compare and contrast the four types of immunologically mediated (hypersensitivity) disorders and give examples of each. Describe clinical features, antigens, mediators, cells and tissues involved
- Compare and contrast the following types of type II hypersensitivity reaction:
- complement dependent
- antibody dependent cell mediated cytotoxicity
- antibody mediated cellular dysfunction
- Compare and contrast acute serum sickness and Arthus reaction.
- Compare and contrast delayed-type hypersensitivity and T cell-mediated cytotoxicity.
- Compare and contrast the following types of transplant rejection:
- hyperacute rejection
- acute rejection
- chronic rejection
- Discuss bone marrow transplantation in terms of:
- indications
- acute and chronic graft vs. host disease
- pathogenesis
- clinical presentation
- complications
- Compare and contrast renal, heart and liver transplants in terms of general morphology of hyperacute rejection, acute rejection and chronic rejection, and other complications.
- Discuss the following disorders:
- systemic lupus erythematosus (SLE)
- discoid lupus erythematosus (DLE)
- drug-induced lupus erythematosis
- Sjögren syndrome
- systemic sclerosis (scleroderma)
- CREST syndrome
- dermatomyositis
- polymyositis
- rheumatoid arthritis (RA)
- juvenile rheumatoid arthritis (JRA)
- ankylosing spondylitis
- Reiter syndrome
- mixed connective tissue disease
- polyarteritis nodosa.
- Compare and contrast the five patterns (classes) of lupus nephritis, in terms of:
- terminology
- relative frequency
- morphology (light, immunofluorescent, and electron microscopic)
- clinical features
- prognosis
- Correlate these patterns of immunofluorescent staining for antinuclear antibodies with the specific antibody represented by each, and disease(s) associated with each:
- homogeneous (diffuse)
- rim (peripheral)
- speckled
- nucleolar
- Match these autoantibodies with theautoimmune disease(s) with which it is associated:
|
- anti-SS-A (Ro) and anti-SS-B (La)
|
|
|
|
|
|
|
|
|
-
Compare and contrast the following immune deficiency syndromes:
- X-linked agammaglobulinemia of Bruton
- common variable immunodeficiency
- DiGeorge syndrome (thymic hypoplasia).
- severe combined immunodeficiency syndrome.
- Wiskott-Aldrich syndrome
- C2 deficiencies
- deficiency of C1 inhibitor (hereditary angioedema)
- chronic granulomatous disease
- myeloperoxidase deficiency
- Discuss secondary immunodeficiency syndromes in terms of etiologies.
- Discuss acquired immunodeficiency syndrome (AIDS), in terms of:
- definition and diagnostic criteria
|
|
|
- associated infections and neoplasms
|
|
|
|
|
|
- complications and prognosis
|
|
|
|