Website assignments:
Additional case (NOT assigned):
Gross specimen videos:
| Organ |
Diagnosis |
Video |
| Colon |
Adenocarcinoma |
Video |
| Colon |
Crohn disease |
Video |
| Colon |
Diverticulosis |
Video |
| Colon |
Ulcerative colitis |
Video |
| Stomach |
Diffuse gastric adenocarcinoma (linnitis plastica) |
Video |
| Stomach |
Intestinal-type gastric adenocarcinoma |
Video |
CASE NUMBER 129
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 70-year-old man was referred to a gastroenterologist due to a six-month history of slowly worsening dysphagia. Esophagogastroduodenoscopy was performed and revealed a friable, necrotic, ulcerated mass. An esophagectomy was performed.
129-1. What is the differential diagnosis?
--ANSWER--
Image Gallery:
Review Esophageal Histology
Slide UCSF 226 (esophagus, H&E)
DigitalScope
Slide UMich 126 40x (trachea & esophagus, H&E)
DigitalScope
Slide UMich 153 20x (esophagus, H&E)
DigitalScope
Slide UMich 155 40x (gastro-esophageal junct, H&E)
DigitalScope
For the purpose of histological descriptions, the esophagus is subdivided into upper (entirely skeletal muscle in the muscularis externa), middle (mixed smooth and skeletal muscle) and lower (entirely smooth muscle) portions. Slide UCSF 226 is from the upper 1/3; slides 126 and 153 are from the middle 1/3; and slide 155 is from the lower 1/3 (at the esophageal-cardiac junction). The esophageal epitheliumis the non-keratinized stratified squamous type and is supported by a connective tissue lamina propria. Note the presence of isolated lymphoid nodules and scattered leukocytes in the lamina propria. A rather thick layer of longitudinally arranged smooth muscle fibers form the muscularis mucosae. The connective tissue of the submucosa consists of mostly collagenous fibers with some elastic fibers and varying amounts of fat as well as submucosal sero-mucous glands which can be readily observed in both slide 126 and slide 153 (those in slide 155 are not very well preserved).
In the upper esophagus, as shown in Slide UCSF 226, the muscularis externa consists of both inner and outer layers of skeletal muscle only. In the middle esophagus, the muscularis externa contains a mixture of skeletal and smooth muscle as seen in slide 126, whereas in the lower esophagus only smooth muscle is found as seen in slide 155. Present in all regions of the esophagus (upper, mid, and lower) is the myenteric (Auerbach’s) plexus between the two layers of the muscularis externa (W pg 267, 14.3). For most of its extent, the esophagus is retroperitoneal, so its outermost layer consists of a connective tissue adventitia which merges with the adjacent connective tissue associated with nearby structures (such as the trachea as shown in slide 126). Below the diaphragm, however, the esophagus is suspended within abdominal cavity and is therefore covered by a connective tissue serosa as shown in slide 155.
|
|
Summary of Gross Findings
The resected esophagus contained a firm, raised, pink-gray, friable and necrotic 3.5 x 4.5 cm tumor mass, completely encircling the esophagus and producing a marked stenosis.
This esophagus has been opened such that the inside of the esophagus is visible, and we are looking at the mucosal surface; the tumor has been carefully left intact and undisrupted (this makes it MUCH easier to measure). Note the erythematous appearance of the tumor in this image – it is likely irritated due to the trauma of swallowing food and liquids. You can imagine as this mass grows into the lumen of the esophagus that it would narrow the diameter of the lumen and potentially obstruct it entirely.
Due to its proximity to vital structures in the mediastinum and thorax, there is a risk of local extension/invasion into nearby structures such as the trachea, aorta, or pericardium.
|
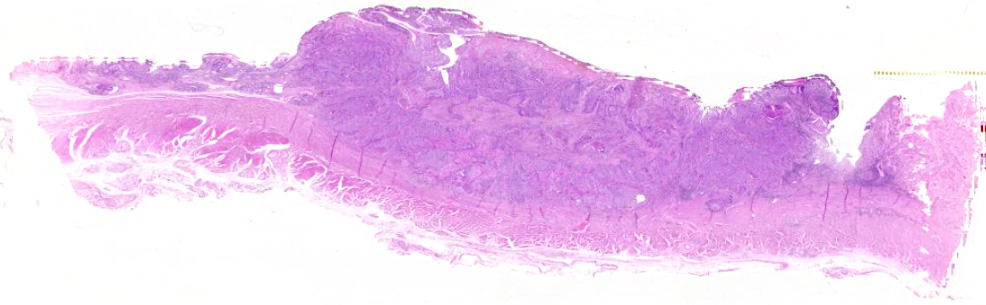
Summary of Microscopic Findings
At one end of the section the squamous epithelium of the esophagus shows marked atypia, pleomorphism and loss of polarity, but no submucosal invasion. These changes represent carcinoma in situ. By following the mucosal lining, one comes upon an area where the cords and nests of poorly differentiated squamous cells are seen to invade the mucosa and submucosa reaching the muscular layer. At one margin of the section the tumor cells are better differentiated with production of keratin and formation of so-called epithelial pearls. Associated with the tumor are marked fibrous proliferation and intense chronic inflammatory infiltration in the stroma. The tumor invades into, but not through the muscularis externa.
|
Gross image questions:
- Describe the gross findings.
- Take a screenshot and annotate where the pathologist should section to confirm that the surgical margins are negative.
VM image questions:
- Describe the VM findings.
- Take a screenshot and identify a keratin pearl (hint: look in the more necrotic area).
129-2. Which of the following is the most significant risk factor for developing this disease?
- Alcohol and tobacco use
- Barrett esophagus
- Gastroesophageal reflux disease
- Helicobacter pylori infection
- PTEN mutation
--ANSWER--
129-3. Intestinal metaplasia (Barrett esophagus) at the gastroesophageal junction is most closely associated with which of the following esophageal lesions?
- Adenocarcinoma
- Eosinophilic esophagitis
- Esophageal varices
- Squamous cell carcinoma
- Squamous papilloma
--ANSWER--
CASE NUMBER 253
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 60-year-old woman was referred to a gastroenterologist due to a one-year history of weight loss with new onset abdominal pain. Physical exam revealed occult blood present in her stool. Upper endoscopy showed a fungating, ulcerated mass in the gastric antrum and the patient underwent a partial gastrectomy. Gross and microscopic images are provided.
253-1. What is the differential diagnosis?
--ANSWER--
Image Gallery:
Review Gastro-Duodenal Histology
Norm No. 16 Stomach, fundus
DigitalScope
Slide UCSF 242 40x (pyloro-duodenal junction, H&E)
DigitalScope
Slide UMich 162 40x (pyloro-duodenal junct, H&E) DigitalScope
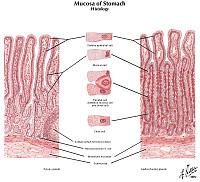
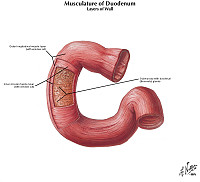
In these slides, you can see the transition from pylorus of the stomach to duodenum of the small intestine. The pyloric region of the stomach is characterized by a thick wall due to the presence of the pyloric sphincter muscle, which is comprised primarily of the inner circular layer of the muscularis externa. Compare its wall thickness with that of the adjacent duodenum. The pyloric glands at the base of each gastric pit [ORIENTATION] are also composed again of a mostly HOMOGENEOUS population of mucous cells that are similar in appearance to those in cardiac glands although the pits are much deeper compared to cardiac glands. Present, but not seen, are stem cells and endocrine cells. An occasional parietal cell may be also found. Note that the bases of the pyloric glands abut the muscularis mucosae whereas in the duodenum, you will see abundant glands (Brunner’s glands) DEEP to the muscularis mucosae (i.e. in the SUBMUCOSA).
|
|
Summary of Gross Findings
The resected portion of the stomach showed a large fungating, partially ulcerated tumor mass in the antrum. Regional lymph nodes and a liver biopsy were free of tumor.
|
Summary of Microscopic Findings
There is a rather abrupt change of the normal stomach mucosa to malignant tumor tissue, projecting into the lumen as a cauliflower-like mass. The tumor forms abundant irregular acini, lined by one or more layers of atypical cells with mostly large irregular nuclei and poorly defined eosinophilic cytoplasm. Atypical mitoses are moderately frequent. The tumor has infiltrated through the muscularis mucosa and the edematous submucosa and has invaded the muscle layers. The invading tumor had elicited a rather marked neutrophilic and plasma cell response.
|
Gross image questions:
- Describe the gross specimen.
- How does this gross appearance DIFFER from that seen in peptic ulcer disease and diffuse gastric adenocarcinoma?
VM image questions:
- Describe the VM findings.
- Take a screenshot and annotate: the gastrointestinal layers (e.g., mucosa, submucosa) and an area of cribriform glands.
- Which is the deepest GI layer into which the tumor invades?
253-2. Which of the following risk factors has the most significant association with this disease?
- Chronic excessive alcohol use
- Cigarette smoking
- Helicobacter pylori infection
- Nitrites from nitrates in food and water
- Ulcerative colitis
--ANSWER--
253-3. Germline mutations in which of the following genes are associated with development of this tumor?
- APC
- CDHI
- KRAS
- MAML2
- NOD2
--ANSWER--
253-4. Infection with which of the following is associated with the development of this disease?
- Candida albicans
- Epstein-Barr virus
- Escherichia coli O157:H7
- Herpes simplex virus type 1
- Human papillomavirus
--ANSWER--
253-5. Metastasis of this tumor to a supraclavicular lymph node is called which of the following?
- Horner syndrome
- Krukenberg tumor
- Pancoast tumor
- Sister Mary Joseph nodule
- Virchow node
--ANSWER--
CASE NUMBER 111 (slide 33748 courtesy of UMich)
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 31-year-old woman with a ten-year history of bloody diarrhea that was adequately managed by immunosuppressant therapy presented to her primary care physician with worsening symptoms. She underwent a colectomy. Gross and microscopic images are provided.
111-1. What is the differential diagnosis?
--ANSWER--
Image Gallery:
Review Colon Histology
Norm No. 27 Colon
[DigitalScope]
The colon is lined by glandular epithelium with numerous mucin secreting goblet cells. The epithelium is infolded into straight tubular glands of uniform diameter to increase the surface area available for secretion and absorption.
|
|
Summary of Gross Findings
The mucosa showed an area of edema and hyperemia distally. This was sharply demarcated from the remainder of the colon. A superficial mucosal lesion was noted.
|
Summary of Microscopic Findings
This section shows fulminant ulcerative colitis with areas of ulceration extending into the submucosa and also some areas of hemorrhage. While deep ulceration is seen, there is no fissuring necrosis, fibrous expansion of the submucosa, or transmural chronic inflammation, which differentiates this lesion from Crohn disease. The base of the ulcerated areas is covered by necrotic debris and fibrinopurulent or sanguinous exudate. Glands are distorted in shape and lined by regenerating epithelium. There are rare crypt abscesses and focal cryptitis.
|
Gross image questions:
- Describe the gross findings and compare and contrast with the gross findings in case 133.
- Take a screenshot and annotate: the lesion, normal colonic mucosa, the proximal surgical margin and the distal surgical margin.
VM image questions:
- Describe the VM findings and compare and contrast with the VM findings in case 133 – use screenshots in your answer.
- Take a screenshot and annotate the layers of gastrointestinal wall.
- Which layers are involved by the lesion?
111-2. Which of the following findings is most supportive of this diagnosis?
- Noncaseating granulomas
- Perianal fistula
- Rectal disease progressing proximally
- Strictures
- Transmural inflammation
--ANSWER--
111-3. Which of the following is more common in this disease than in other types of inflammatory bowel disease?
- Ankylosing spondylitis
- Erythema nodosum
- Migratory polyarthritis
- Primary sclerosing cholangitis
- Uveitis
--ANSWER--
111-4. Which of the following is associated with partial relief of symptoms in patients with this disease?
- Ciprofloxacin
- Clostridium difficile infection
- Estrogen therapy
- Radiation
- Smoking
--ANSWER--
111-5. Which of the following is most accurate regarding colitis-associated neoplasia in patients with this disease?
- Degree of dysplasia is associated with extent of granuloma formation
- Incidence is greatest in patients with left-side only colitis
- Increased active disease is associated with lower risk
- Primary sclerosing cholangitis is associated with increased risk
- Risk increases sharply 5 years after disease initiation
--ANSWER--
CASE NUMBER 84 (slide 9849 courtesy of University of Leeds)
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 64-year-old woman presented to her primary care physician with a six-month history of weakness and weight loss and recent onset colicky abdominal pain and distention. She also stated that she had noticed some blood in her stool. Physical exam revealed occult blood in her stool and a mass was palpated in the rectum. The patient underwent an abdominoperineal resection. Gross and microscopic images are provided.
84-1. What is the differential diagnosis?
--ANSWER--
Image Gallery:
Review Colon Histology
Norm No. 27 Colon
[DigitalScope]
The colon is lined by glandular epithelium with numerous mucin secreting goblet cells. The epithelium is infolded into straight tubular glands of uniform diameter to increase the surface area available for secretion and absorption.
|
|
Summary of Gross Findings
There is a circumferential mass approximately 6 cm from the anus that causes luminal narrowing. The bowel wall at this site is thickened and appears fibrotic. The colon proximal to the lesion is dilated.
|
Summary of Microscopic Findings
This section of colonic mucosa shows an invasive adenocarcinoma that is diffusely infiltrating into but not through the muscularis propria. Lymphvascular invasion is not seen. The lumina of the glands shows the characteristic “dirty necrosis” seen in colorectal carcinoma. This microscopic section does not show the extensive desmoplasia suggested by the gross appearance.
|
Gross image questions:
- Describe the gross specimen.
- Take a screenshot and annotate: the proximal and circumferential surgical margins and the tumor.
- What accounts for the proximal colonic dilation?
VM image questions:
- Describe the VM findings. Into which layer is the tumor invading?
- Take a screenshot and identify the invasive component as well as an intramucosal component.
84-2. Which of the following is the most important prognostic indicator for this disease?
- Depth of invasion
- Number of mitotic figures
- Presence of necrosis
- Tumor diameter
- Tumor site
--ANSWER--
84-3. Which of the following is the gene that is usually the first to be mutated in the adenoma-carcinoma progression?
- APC
- KRAS
- P53
- SMAD2
- Telomerase
--ANSWER--
84-4. Increased consumption of which of the following is associated with decreased risk of this disease?
- Alcohol
- Aspirin
- Coffee
- Red meat
- Saturated fats
--ANSWER--
84-5. Which of the following is the most common clinical presentation for a right-sided colonic adenocarcinoma?
- Constipation
- Cramping epigastric pain
- Diarrhea
- Iron deficiency anemia
- Nausea and vomiting
--ANSWER--
CASE NUMBER 133
[DigitalScope]
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 39-year-old man presented to his gastroenterologist with a one-day history of cramping, lower abdominal pain and bloating that he noticed about five hours after a meal. He also reported bloody diarrhea. His clinical history is significant for an 8-year history of enteritis and a one-year history of a non-healing rectal fistula. Large bowel obstruction was suspected and he underwent a partial colon resection. Gross and microscopic images are provided.
133-1. What is the differential diagnosis?
--ANSWER--
Image Gallery:
Review Colon Histology
Norm No. 27 Colon
[DigitalScope]
The colon is lined by glandular epithelium with numerous mucin secreting goblet cells. The epithelium is infolded into straight tubular glands of uniform diameter to increase the surface area available for secretion and absorption.
|
|
Summary of Gross Findings
The colon showed extensive ulcerations separated by pedunculated areas of hypertrophic mucosa. The intestinal wall was swollen and edematous. The serosa was thickened with fibrous adhesions.
|
Summary of Microscopic Findings
There are broad areas of ulceration extendint into the submucosa. The surface of the ulcers is covered by fibrinopurulent exudate overlying granulation tissue. Neutrophils infiltrate glands in the adjacent mucosa, some of which are lined by regenerating epithelium. A few crypts are distorted in shape and crypt abscesses are present. These features differ little from those seen in ulcerative colitis ( Case No. 111). However, this section also shows transmural chronic inflammation in the form of lymphoid aggregates and granulomatous inflammation. |
133-2. Which of the following is most commonly seen in this disease?
- Abundant pseudopolyps
- Rectal involvement
- Superficial ulceration
- Toxic megacolon
- Transmural inflammation
--ANSWER--
GI SYSTEM Review Items
Key Vocabulary Terms (click here to search any additional terms on Stedman's Online Medical Dictionary)
LEARNING OBJECTIVES - Gastrointestinal Tract Pathology
Goal 1: Embryology of the Gut
Apply knowledge of the embryology of the foregut, midgut and hindgut to summarize the morphological features and clinical presentation of developmental anomalies.
Objective1.1: Congenital Disorders of the Gut
Outline the clinicopathological features of tracheoesophageal fistula, pyloric stenosis, intestinal atresia, and Hirschprung diseases.
Goal 2: Anatomy and Blood Supply of the Gut
Apply knowledge of the gross anatomy of the GI tract and hemodynamic principles to discuss vascular disorders.
Objective 2.1: Ischemic Disorders of the Gut
Outline the pathogenesis and clinicopathological features for common disorders of the GI tract that arise from hypoxia or ischemia.
Goal 3: Gastrointestinal Neoplasia
Apply knowledge of the molecular basis of neoplasia to explain the clinical presentation, inheritance risk, biologic behavior, morphologic appearance, classification, diagnosis, prognosis and targeted therapy of gastrointestinal neoplasms.
Objective 3.1: Precursors to Bowel Carcinoma
Outline the precursor lesions, risk factors, and hereditary cancer syndromes that lead to GI neoplasia.
Objective 3.2: Molecular Basis of Bowel Neoplasms
Summarize the molecular basis and clinicopathologic features, local and systemic, for esophageal cancer, gastric cancer, GI lymphoma, GIST, colon and anal cancer.
Objective 3.3: Esophageal Carcinoma
Describe the location of adenocarcinomas versus squamous cell carcinomas of the esophagus and list the major risk factors for each.
Objective 3.4 Gastric Polyps
Compare and contrast the different types of gastric polyps in terms of risk factors, etiology, clinical presentation, histologic findings, treatment and risk for malignant transformation.
Objective 3.5 Gastric Carcinoma
Compare and contrast the different types of gastric carcinoma in terms of risk factors, epidemiology, etiology, clinical presentation, histologic findings, prognosis and treatment.
Objective 3.6: Colonic Polyps
Describe the different types of polyps and the risk of developing cancer.
Objective 3.7: Colon Carcinoma
List the most important prognostic factors for colon cancer and explain why they are most important.
Goal 4: Features of Gastrointestinal Neoplasms
Apply knowledge of the gross anatomy of the GI tract and its blood supply to describe presenting signs and symptoms, and pattern of spread of gastrointestinal neoplasms.
Objective 4.1: Right- and Left-sided Colon Carcinoma
Distinguish between carcinomas arising in the left and right colon in terms of symptoms and morphology.
Objective 4.2: Staging of Colon Carcinoma
Describe how colon cancers are staged and list the common sites of metastases.
Goal 5: Immune-Related Disorders of the Bowel
Apply knowledge of immune system dysregulation to discuss specific immune-related disorders.
Objective 5.1: Inflammatory Bowel Disease
Compare and contrast the pathophysiology and clinicopathological features of inflammatory bowel disease.
Objective 5.2: Celiac Disease
Explain the pathophysiology of gliadin hypersensitivity (Celiac disease).
Goal 6: Malabsorption
Apply knowledge of gastrointestinal anatomy and physiology to summarize the clinicopathologic features, diagnostic criteria, and therapy of disorders presenting with malabsorption.
Objective 6.1: Pancreaticobiliary Causes of Malabsorption
Outline disorders of the pancreas and bile acid metabolism, and discuss how they lead to malabsorption.
Objective 6.2: Inflammatory Causes of Malabsorption
Explain how Celiac disease, sprue, gastroenteritis, and inflammatory bowel disease lead to malabsorption.
Goal 7: Bowel Infections
Apply knowledge of common pathogens and principles of immunity to describe the morphological features and clinical presentation of infectious diseases affecting immunocompetent and immunocompromised patients.
Objective 7.1: Bowel Infections
Compare the underlying mechanism and clinicopathologic features of GI tract involvement by common bacterial, fungal and parasitic pathogens.
Objective 7.2: Helicobacter Infection
Relate the clinicopathologic features of Helicobacter to chronic gastritis and ulcer formation.
Goal 8: Mechanical Disorders of Bowel
Apply knowledge of GI anatomy and physiology to explain the clinicopathologic features, diagnostic criteria and therapy of disorders resulting in acid reflux, abnormal GI motility and gastrointestinal tract obstruction.
Objective 8.1: Dysphagia
Describe the pathophysiology and clinicopathological features of disorders presenting with dysphagia.
Objective 8.2: Bowel Obstruction
Compare and contrast the pathophysiology of gastrointestinal disorders that present with GI obstruction.
Objective 8.3: Diverticulosis
Describe the complications of diverticulosis.
|