Website cases
Additional case (NOT assigned):
Gross specimen videos:
| Organ |
Diagnosis |
Video |
| Liver |
Cirrhosis |
Video |
| Liver |
Primary hepatocellular carcinoma |
Video |
| Liver |
Metastatic carcinoma |
Video |
| Pancreas |
Pancreatic adenocarcinoma |
Video |
| Pancreas |
Acute pancreatitis (w/ fat necrosis) |
Video |
| Gallbladder |
Cholelithiasis |
Video |
CASE NUMBER 521
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 35-year-old man presents to the emergency department with a 2-week history of fever and jaundice. Physical exam reveals a thin man with skin lesions on his left arm.
521-1a. What is the differential diagnosis based on the clinical presentation?
--ANSWER--
Image Gallery:
The clinical image shows injection marks, consistent with IV drug use.
|
|
521-2. Which tests would you order?
--ANSWER--
Clinical history, part 2 (click here to open)
Clinical history, part 3 (click here to open)
CASE NUMBER 27
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 40-year-old man with a longstanding history of mild ulcerative colitis presents to his primary care physician with a 3-month history of fatigue and intermittent upper abdominal pain. Laboratory values show the following:
- serum alkaline phosphatase 350 U/L (normal 30-135 U/L)
- AST of 180 U/L (normal 10 – 60 U/L)
- ALT of 360 U/L (normal 10 – 60 U/L)
- Bilirubin is normal (<1.2 mg/dL)
Endoscopic retrograde cholangiopancreatography (ERCP) was performed, followed by a biopsy. Over the next five years, the patient's disease progressed and he underwent a liver transplant.
27-1a. What is the differential diagnosis based on the initial presentation?
27-1b. How do the laboratory tests contribute to the differential diagnosis?
27-1c. What is the final diagnosis?
--ANSWER--
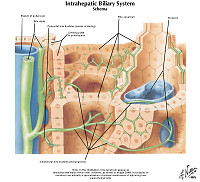
Virtual Slide and Image Gallery:
Slide (UMich _30868):
[DigitalScope]
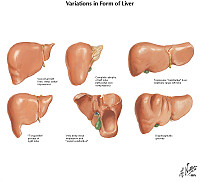
Review Liver Histology
Slide 3: Liver
[DigitalScope]
The liver is the organ that metabolizes nutrients received from the digestive tract. These nutrients and processed by tissue hepatocytes which are large polygonal cells. The hepatocyes are separated by portal triads. The triads consist of an artery, a vein and a bile duct. The bile duct is lined by cuboidal epithelium. The artery has a muscular wall and a flat endothelial lining. The sinuses are well defined and contain a small amount of blood.
|
|
Summary of Imaging Findings
Endoscopic retrograde cholangiopancreatography shows the characteristic beading appearance due to areas of mild dilation interspersed with areas of stricture caused by fibrosis.
|
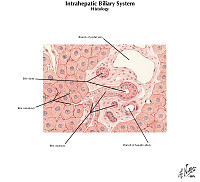
Summary of Microscopic Findings
This section of liver shows periductal fibrosis, ductal proliferation and mild chronic inflammation.
|
Radiology image questions:
- Describe the radiologic findings. What would be your differential diagnosis based on the radiologic findings?
VM image questions:
- Describe the histologic findings.
- Take a screenshot and annotate: an area of onion-skin fibrosis, inflammation and pigmented macrophages.
- Which type of inflammatory cells is present?
- What is the pigment in the macrophages?
- How do the histologic findings correlate with the radiologic findings?
27-2. Which of the following is most closely associated with this disease?
- Anti-cyclic citrullinated peptides
- Anti-mitochondrial antibodies (AMA)
- Anti-nuclear antibody (ANA)
- Anti-phospholipid antibody
- Anti-neutrophil cytoplasmic antibodies (ANCA)
--ANSWER--
27-3. Which of the following is MOST ACCURATE about this disease?
- Approximately 70% of patients have Crohn disease
- Mutations in RB are seen in 25% of patients
- Patients have an increased risk of cholangiocarcinoma
- Ursodeoxycholic acid slows disease progression
- Women are twice as likely to be affected as men
--ANSWER--
CASE NUMBER 189
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 60-year-old man presented to his primary care physician with a 6-month history of intermittent abdominal pain. During the past three weeks, he had noticed chalky and greasy stools and that he felt itchy. Clinical history revealed an unintentional 20-pound weight loss over the previous two months that he attributed to decreased appetite. Physical exam showed icterus. MRI revealed a mass in the head of the pancreas and the patient underwent surgical resection of this mass. Gross and microscopic images are provided.
189-1a. What is the differential diagnosis based on initial presentation?
189-1b. How does the imaging focus the differential diagnosis?
189-1c. What is the final diagnosis?
--ANSWER--
Virtual Slide and Image Gallery:
Slide (UMich 103): [DigitalScope]
Review Pancreas Histology
Norm No. 7 Pancreas
[DigitalScope]
The pancreas is comprised of glandular tissue with endocrine and exocrine function. The exocrine pancreas contains lobular arrays of acini. The acinar secretions of the exocrine pancreas are collected by the pancreatic ducts. The ducts are surrounded by a small amount of connective tissue without inflammation or fibrosis (scarring). The endocrine pancreas resides in the islets which are regularly arranged and present within the pancreatic lobules.
|
|
Summary of Gross Findings
The head of the pancreas was enlarged with yellow-gray firm tissue, in which no normal lobular structures were seen. About 4 cm proximal to the ampulla there was a stenosis of the common bile duct. Proximal to this stenosis the bile ducts were markedly dilated with bile. The peripancreatic lymph nodes and the celiac axis were gray and firm with metastastic tumor.
|
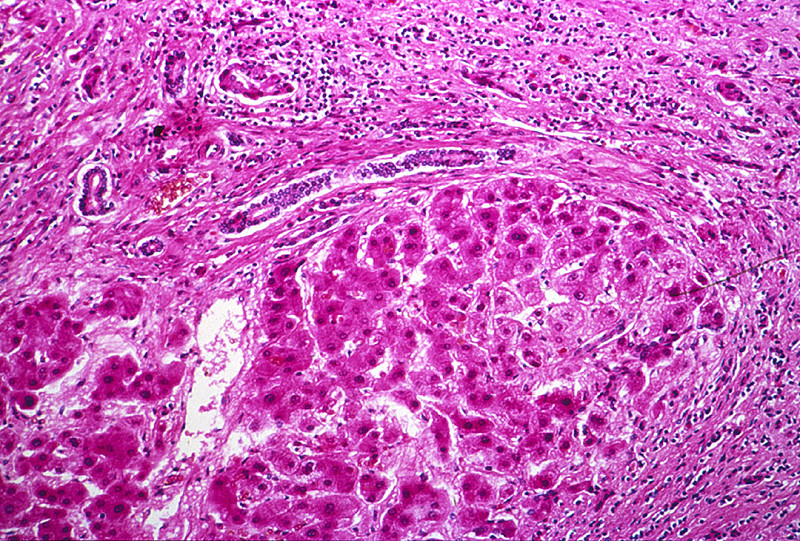
Summary of Microscopic Findings
The tumor is composed of duct-like structures, which are irregularly arranged and infiltrate into the dense connective stroma and perivascular or perineural lymphatics. Occasionally both ducts and individual tumor cells contain mucin. There is a small amount of pancreatic tissue which shows marked atrophy and fibrosis. The small ducts are distended and may show focal squamous metaplasia of the epithelium in some sections.
|
Gross image questions:
- Describe the gross appearance.
- Which part of the intestine is shown in the gross image?
- Take a screenshot and identify: the lesion and the ampulla of Vater.
VM image questions:
- Describe the histologic findings.
- Take a screenshot and annotate: an islet of Langerhans, desmoplasia and cribriform architecture.
- Does this appear to be an aggressive tumor? Why or why not?
189-2. Which of the following is most commonly mutated in this disease?
- BRCA2
- GNAS
- KRAS
- SMAD4
- VHL
--ANSWER--
189-3. Which of the following is usually a precursor lesion for this disease?
- Acute pancreatitis
- Chronic pancreatitis
- Pancreatic intraepithelial neoplasia
- Pancreatic pseudocysts
- Serous cystadenoma
--ANSWER--
189-4. Which of the following is most closely associated with this disease?
- Budd-Chiari syndrome
- Cystic fibrosis
- Hypercalcemia
- Increased serum IgG4
- Migratory thrombophlebitis
--ANSWER--
CASE NUMBER 93
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 50-year-old man with a history of alcohol use disorder presented to the emergency department with severe epigastric pain that radiated to his back. He stated that he had had multiple similar episodes over the previous five years and had been hospitalized several times for pain management. At this admission, laboratory analysis showed elevated levels of serum lipase. The patient developed refractory shock, peritonitis and died. Gross and microscopic images from the autopsy are provided.
93-1a. What is the differential diagnosis based on the clinical history and initial presentation?
93-1b. How do the laboratory tests contribute to the differential diagnosis?
93-1c. What is the final diagnosis?
--ANSWER--
Virtual Slide and Image Gallery:
Slide 0093_Q: [DigitalScope]
Review Pancreas Histology
Norm No. 7 Pancreas
[DigitalScope]
The pancreas is comprised of glandular tissue with endocrine and exocrine function. The exocrine pancreas contains lobular arrays of acini. The acinar secretions of the exocrine pancreas are collected by the pancreatic ducts. The ducts are surrounded by a small amount of connective tissue without inflammation or fibrosis (scarring). The endocrine pancreas resides in the islets which are regularly arranged and present within the pancreatic lobules.
|
|
Summary of Gross Findings
In this specimen, the stomach is reflected superiorly and the spleen can be is visible at the far upper right. The pancreas is edematous with areas of hemorrhage. Classic features of fat necrosis are not seen.
|
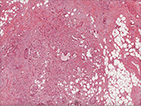
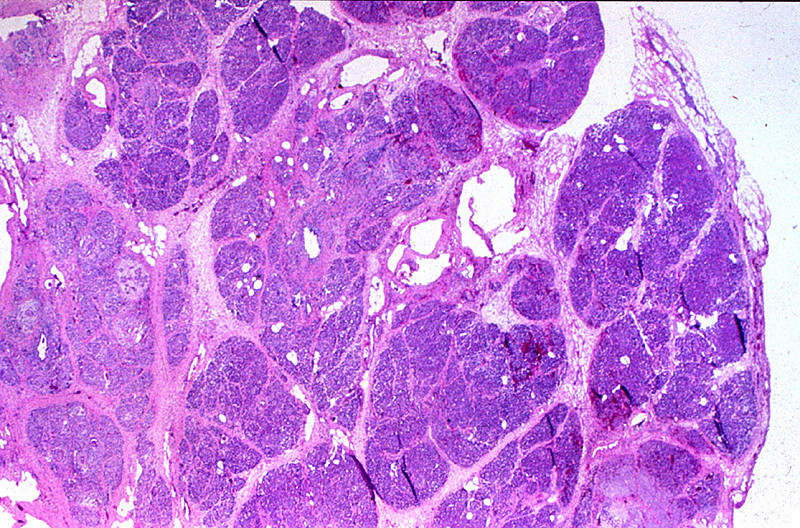
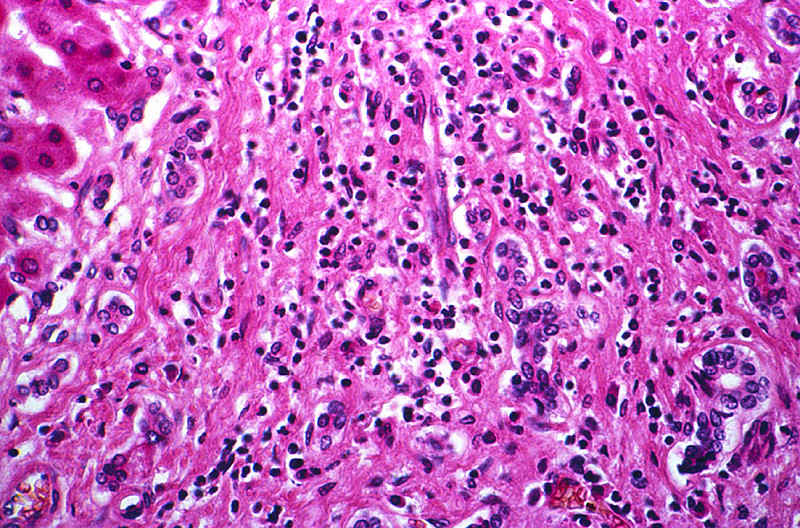
Summary of Microscopic Findings
Several areas of fat necrosis with adjacent neutrophil infiltrate are seen, evidence of acute pancreatitis. In addition, some lobules of the pancreas show fibrosis and loss acini, evidence of chronic pancreatitis. In these areas, islets of Langerhans appear larger and more abundant. This is partly because they are resistant to injury and persist when acini are destroyed and partly because they undergo reactive hyperplasia.
|
Gross image questions:
- Describe the gross findings of the pancreas.*
*note: This gross image is a bit difficult to orient. The stomach has been reflected upwards; the central part of the image is the pancreas. In the upper right is a portion of spleen.
VM image questions:
- Describe the histologic findings.
- Take a screenshot and annotate: an islet, an area of fibrosis, fat necrosis, hemorrhage and parenchymal necrosis.
93-2. Which of the following is the most common cause of this disease?
- Cystic fibrosis
- Excessive alcohol use
- Annular pancreas
- Pancreas divisum
- SPINK1 mutation
--ANSWER--
93-3. Which of the following is the most likely sequela of this disease?
- Adenocarcinoma of the pancreas
- Aortic dissection
- IgG4 inflammatory disease
- Metastatic calcification
- Pancreatic pseudocyst
--ANSWER--
93-4. Which of the following laboratory values is usually the first to increase in this disease?
- Serum amylase
- Serum calcium
- Serum lipase
- Urinary ketones
- White blood cell count
--ANSWER--
CASE NUMBER 81
--Click here for a video debrief of the pathology findings presented in this case--
Clinical History: A 62-year-old man with a history of chronic alcohol use disorder presented to his primary care physician with a 3-month history of increased abdominal girth. Physical exam revealed telangiectasias and fluid wave of the abdomen. Laboratory findings showed elevated aminotransferase and decreased serum albumin; no other significant findings were noted. He was admitted to the hospital for further evaluation, but began retching violently with extensive hematemesis. Volume resuscitation failed and the patient died. Gross and microscopic images from the autopsy are provided.
81-1. What is the differential diagnosis?
--ANSWER--
Virtual Slide and Image Slide Gallery:
Slide 0081_Q: [DigitalScope]
Review Liver Histology
Slide 3: Liver
[DigitalScope]
The liver is the organ that metabolizes nutrients received from the digestive tract. These nutrients and processed by tissue hepatocytes which are large polygonal cells. The hepatocyes are separated by portal triads. The triads consist of an artery, a vein and a bile duct. The bile duct is lined by cuboidal epithelium. The artery has a muscular wall and a flat endothelial lining. The sinuses are well defined and contain a small amount of blo |
|
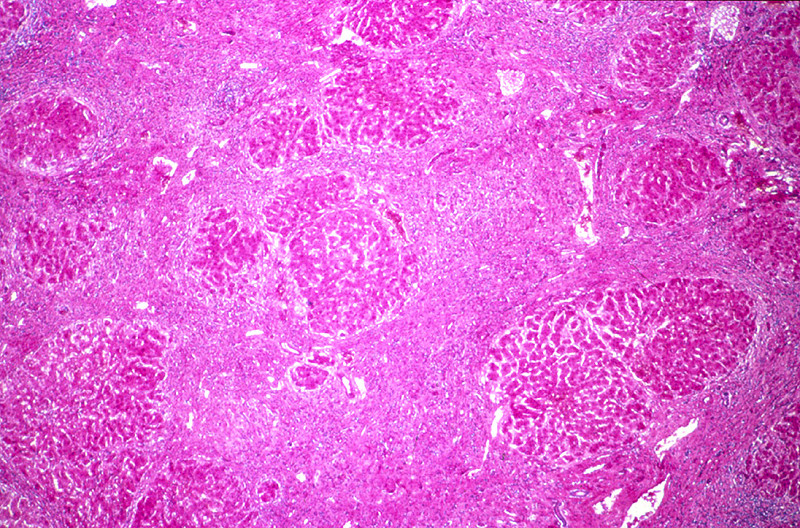
Summary of Gross Findings
The liver weighed 1800 grams. The entire organ was uniformly composed of nodules about 0.5 cm in diameter, each surrounded by fibrous tissue. The organ was jaundiced and firm.
|
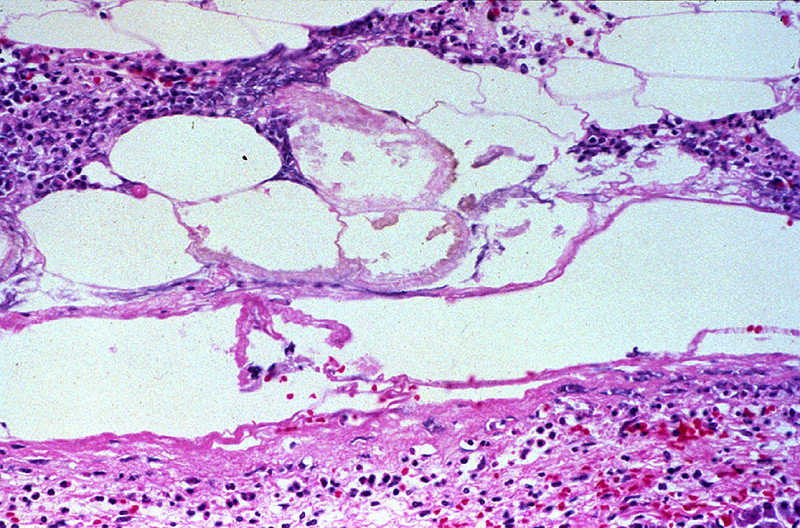
Summary of Microscopic Findings
The usual architecture present in the liver has been completely disrupted by the bands of connective tissue. In these bands one sees chronic inflammatory cells, mainly lymphocytes and other mononuclear cells. There is some proliferation of the bile ductules.
| -->
81-2. Which of the following is the most common cause of this disease?
- Chronic alcohol use disorder
- Hepatitis B
- Hemachromatosis
- Non-alcoholic fatty liver disease
- Wilson disease
--ANSWER--
81-3. Mallory bodies are intracytoplasmic accumulations of which of the following?
- Cytokeratin
- Desmin
- GFAP
- Glycogen
- Lipid
--ANSWER--
81-4. A patient with identical gross and microscopic findings is identified. However, his liver shows intracytoplasmic globules that are periodic acid-Schiff positive as shown below:
- Which of the following additional findings would you expect?
- Anti-nuclear antibodies (ANAs)
- Decreased levels of serum ceruloplasmin
- Hepatic vein thrombosis
- PiZZ genotype
- Polycystic kidney disease
--ANSWER--
LIVER and BILIARY TRACT Review Items
Key Vocabulary Terms (click here to search any additional terms on Stedman's Online Medical Dictionary)
LEARNING OBJECTIVES
Goal 1: Hepatitis
Apply knowledge of infectious disease, immune mechanisms, pathogenesis, laboratory profiles, and histopathological patterns of injury to discuss infectious and autoimmune hepatitis.
Objective 1.1: Transmission of Hepatotropic Viruses
Explain the routes of transmission of different hepatotropic viruses and how they relate to the public health measures that have been implemented to prevent their transmission.
Objective 1.2: Progression of Hepatitis
Compare and contrast the possible clinical outcomes of the major hepatotropic viruses with particular reference to the incidence of progression to chronic hepatitis and cirrhosis.
Objective 1.3: Pathophysiology of Hepatitis
Describe the pathophysiology associated with the major hepatotropic viruses and explain how this knowledge can be used to assess the presence of hepatitis, and the management and prognosis of the disease.
Objective 1.4: Histopathology of Hepatitis
Explain the pathogenetic mechanisms of injury that result in the histopathological findings observed in acute and chronic viral hepatitis.
Objective 1.5: Cirrhosis
Classify types of cirrhosis, in terms of etiology, pathogenesis, morphologic pattern (gross and microscopic), and their relationship to neoplasia.
Objective 1.6: Autoimmune Hepatitis
Describe the etiology, clinical presentation, pathologic features, laboratory values and prognosis of autoimmune hepatitis.
Goal 2: Liver Toxins
Apply knowledge of the cellular response to injury, the pathogenic mechanisms leading to disease and the biochemical alterations of hepatic function to explain the clinicopathologic features, prognosis and treatment of disorders resulting from ethanol and other drugs and toxins.
Objective 2.1: Steatosis
Describe the clinicopathologic features of excessive ethanol ingestion, focusing on biochemical pathways and short and long term complications, and contrast them with nonalcoholic fatty liver disease.
Objective 2.2: Acetominophen Toxicity
Describe the clinicopathologic features of excessive acetaminophen ingestion focusing on biochemical pathways and short and long term complications.
Goal 3: Inherited Metabolic Diseases
Apply knowledge of biochemistry, cellular biology and metabolic pathways to describe the metabolic diseases of the liver.
Objective 1: Disorders of Metal Metabolism
Compare and contrast hemochromatosis and Wilson disease in terms of etiology, genetics, clinical presentation, pathologic features and long-term consequences.
Objective 2: Alpha 1 – Anti-Trypsin Deficiency
Describe alpha 1-anti-trypsin deficiency in terms of etiology, genetics, clinical presentation, pathologic features and long-term consequences.
Goal 4: Hepatic Neoplasia
Apply knowledge of the molecular basis of neoplasia to describe the clinical presentation, biologic behavior, morphologic appearance, classification, diagnosis, prognosis and targeted therapy of hepatic neoplasms.
Objective 1: Causes of Hepatocellular Carcinoma
Compare and contrast, in the context of geographic location, the epidemiological importance of the known etiologic agents associated with the development of hepatocellular carcinoma and suggest public health measures that might decrease its incidence.
Objective 2: Pathogenesis of Hepatocellular Carcinoma
Discuss the pathogenesis of hepatocellular carcinoma arising in the setting of hepatitis B and hepatitis C, chronic hepatitis, and cirrhosis.
Objective 3: Benign Hepatic Nodules
Compare and contrast focal nodular hyperplasia and hepatocellular adenoma in terms of clinical presentation, risk factors, pathologic findings and risk for malignant transformation.
Objective 4: Metastasis to the Liver
Describe the factors that lead to metastasis to the liver and the features of metastatic disease that distinguish it from primary neoplasms.
Goal 5: Biliary Tract Neoplasia
Apply knowledge of the cellular response to injury, the pathogenic mechanisms leading to disease and the biochemical alterations of hepatic function to describe the clinicopathologic features, prognosis and treatment of intrahepatic and extrahepatic biliary tract diseases.
Objective 1: Autoimmune Cholangiopathies
Outline how primary biliary cholangitis and primary sclerosing cholangitis differ regarding associated conditions, incidence, sex predilection, etiology, laboratory features, clinical features and prognosis.
Objective 2: Extrahepatic Biliary Carcinoma
Describe the epidemiology, morphology, and clinical features of gallbladder and extrahepatic biliary tract carcinoma.
Objective 3: Cholangiocarcinoma
Describe the presenting symptoms of cholangiocarcinoma and how the symptoms relate to the location.
Goal 7: Cholelithiasis
Apply knowledge of general biochemical principles to an understanding of how gallstones develop, risk factors for their development, and their clinical presentation and complications.
Objective 7.1: Gallstones
Describe the risk factors, clinical features, complications, mechanisms, and composition of gallstones.
Objective 7.2: Cholecystitis
Differentiate the epidemiology, morphology, clinical features, and complications of acute and chronic cholecystitis.
PANCREAS Review Items
Key Vocabulary Terms (click here to search any additional terms on Stedman's Online Medical Dictionary)
LEARNING OBJECTIVES
Goal 8: Nonneoplastic Disorders of the Exocrine Pancreas
Apply knowledge of the structure and function of the pancreas to an understanding of the clinicopathologic features and diagnostic criteria of disorders resulting from cellular injury to the exocrine pancreas.
Objective 1: Pancreatitis
Compare and contrast acute and chronic pancreatitis in terms of etiology, pathogenesis, morphologic features, and complications.
Goal 2: Pancreatic Neoplasia
Apply knowledge of the molecular basis of neoplasia to an understanding of the clinical presentation, biologic behavior, morphologic appearance, classification, diagnosis, prognosis, and targeted therapy of pancreatic neoplasms.
Objective 2.1: Neoplasia of the Pancreas
Describe the major types of neoplasms affecting the exocrine pancreas.
Objective 2.2: Clinical Features of the Pancreatic Adenocarcinoma
Explain how the location of a pancreatic neoplasm determines its presenting symptoms and discuss the risk factors for pancreatic adenocarcinoma.
Objective 2.3: Endocrine Neoplasms of the Pancreas
Describe clinicopathological features of neoplasms of the endocrine pancreas.
|