Case assignments by lab group and class day:
| |
TUESDAY |
THURSDAY |
Labs 1, 2, & 3 |
|
|
Labs 4 & 5 |
|
|
CASE NUMBER 504
(no virtual slide for this case)
Clinical History: A 25-year-old woman presented to her primary care physician with a one-week history of blurred vision in her left eye. She stated that it was painful to move that eye. She grew up in Minnesota and has smoked one-half of a pack of cigarettes/day for the last 7 years. Further questioning reveals that she had unilateral tingling on her left side in the two weeks before her wedding 3 years ago. CSF analysis showed mildly elevated protein and moderate pleocytosis. MRI revealed multiple hypointense lesions and FLAIR (fluid-attentuated inversion recovery) MRI showed multiple supratentorial lesions. When the patient learned of her possible diagnosis, she returned home and took an overdose of sleeping pills. Gross and microscopic images of the autopsy are provided.
Image Gallery:
(Summary of Imaging Findings - click here)
MRI shows multiple white matter lesions in the corpus callosum, subcortical U-fibers, temporal lobes, brainstem, cerebellum and spinal cord.
|
(Summary of Gross Findings - click here)
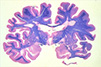
There were multiple well circumscribed somewhat depressed lesions in the white matter. A depressed, tan area representing a sclerotic plaque is seen here adjacent to a cerebral ventricle. A coronal section through the cerebrum has been stained with luxol fast blue/hematoxylin and eosin which stains the myelinated white matter blue and the cortex pink. There are multiple plaques of demyelination.
|
(Summary of Microscopic Findings - click here)
A low power image of a luxol blue-stained section shows a circumscribed demylenated lesion. A high power microscopic image of white matter stained with luxol fast blue & eosin illustrates absence of myelin. The adjacent image stained with Glees silver stain illustrates that individual axons are intact.
|
|
504-1. What is the differential diagnosis?
ANSWER
504-2. The lesions in this disease are caused by an immune response directed against which of the following?
- Amyloid precursor protein
- Aquaporins
- Huntingtin
- Myelin sheath
- Substantia nigra
ANSWER
504-3. The patient has an identical twin. Which of the following MOST CLOSELY approximates her risk for developing the same disease?
- <1%
- 25%
- 50%
- 66%
- 75%
- 100%
ANSWER
504-4. Which of the following is typically seen in the CSF of patients with this disease?
- Abundant red blood cells
- Decreased protein level
- Myelin
- Oligoclonal bands
- PrPsc
ANSWER
CASE NUMBER 543 - slide courtesy of UMich, PhosphoTungstic Acid-Hematoxylin (PTAH) stain
[ImageScope] [WebScope]
Clinical History: A previously healthy 62-year-old man presents to his GP after noticing that his right hand trembles when he was at rest. His wife mentioned that his handwriting had become smaller and that when he walked his right arm swung less than his left. Physical exam revealed decreased facial expression and a reduced blink frequency. In addition, he had cogwheel rigidity bilaterally. Radiologic imaging was unremarkable and laboratory tests were within normal limits. The patient dies in an automobile accident. A section of his midbrain at autopsy is provided.
Imaging: MRI shows mild ventricular dilation. (Images from Meijer FJA, Goraj B (2014). Frontiers in Bioscience E6, 360-369.
Image Gallery:
(Summary of Imaging Findings - click here)
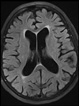
Axial T2 FLAIR MRI shows non-specific cortical atrophy with sulcal widening and enlargement of the lateral ventricles. (Image from Meijer FJA, Goraj B (2014). Frontiers in Bioscience E6, 360-369.)
|
(Summary of Gross Findings - click here)
A coronal section through the midbrain illustrates pallor of the substantia nigra. The midbrain of the patient is displayed on the right. A normal midbrain is shown on the left.
|
(Summary of Microscopic Findings - click here)
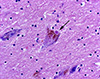
Histologic section of the sustantia nigra shows loss of pigmented neurons with pigment incontinence. Viable pigmented neurons contain eosinophilic cytoplasmic inclusions with a halo.
|
|
543-1. What is the differential diagnosis?
ANSWER
543-2. Which of the following is most likely to be the protein found in the neuronal inclusions seen in figure 3?
- α-synuclein
- Amyloid precursor protein
- Huntingtin
- Superoxide dismutase
- Tau
ANSWER
543-3. Which of the following is a component of first-therapy for this disease?
- Cholinesterase inhibitors
- Gabapentin
- L-DOPA
- Radiation
- Selective serotonin reuptake inhibitor
ANSWER
543-4. Which of the following is the term applied when dementia arises within 1 year of the onset of motor symptoms?
- Central pontine myelinolysis
- Frontotemporal lobar degeneration
- Krabbe disease
- Lewy body dementia
- Pick disease
ANSWER
CASE NUMBER 515
(no virtual slides for this case)
Clinical History: A 46-year-old man with a long history of alcohol abuse was brought to the emergency department by the police when he was found walking unsteadily and seemed confused. His speech was slurred and slow, though his blood alcohol was 0.01%. A mini mental status exam revealed that his short term memory was severely impaired. Physical exam revealed a right leg tremor and nystagmus. A cranial MRI was performed, but while the patient was still in radiology, when the patient tried get off of the gurney, he fell, hit his head on the floor and died.
Image Gallery:
515-1. What is the differential diagnosis?
ANSWER>
515-2. The constellation of symptoms shown by this patient is known as which of the following?
- Kwashiorkor
- Leigh syndrome
- Parkinsonism
- Ricketts
- Wernicke-Korsakoff syndrome
ANSWER
515-3. Which of the following typically develops late in this disease?
- Amnesia
- Ataxia
- Cognitive impairment
- Confusion
- Nystagmus
ANSWER
515-4. Which of the following is true regarding this patient’s symptoms?
- Ataxia rarely improves with appropriate treatment
- Confusion rarely improves with appropriate treatment
- Memory loss typically improves with appropriate treatment
- Nystagmus typically improves with appropriate treatment
ANSWER
515-5. In addition to alcoholism, in which of the following clinical settings is this disease process MOST LIKELY to arise?
- Chronic blood loss
- Gastric disorders
- Inborn error metabolism
- Obesity
- Renal disease
ANSWER
CASE NUMBER 301
Clinical History: A 10 year-old child boy travels with his family on a 4-week “eco-vacation” in Malaysia, backpacking in tropical and semi-tropical forests. They have no direct animal contact, but they are constantly exposed to mosquitos. One day prior to their return to the US, the patient begins to experience headaches, fevers, and chills. During the transcontinental flight, he becomes increasing disoriented and confused. Upon landing, the family rushes him to a local tertiary medical center. He was obtunded on admission.
Clinical History, Part 2 (click here)
Clinical History, Part 3 (click here)
301-1. What is the differential diagnosis?
ANSWER
CASE NUMBER 300
Clinical History: A 14-year-old girl is brought to the emergency department with a 1-day history of fevers and decreased consciousness. She had been well until the previous day when she awoke with left-sided headache, anorexia, fatigue, and subjective fevers. During the course of the day, her level of consciousness decreased. In the ED, her temperature is 38.8°C, and she is difficult to arouse. She resists neck flexion, but the remainder of her physical examination is unremarkable.
Clinical History, Part 2 (click here)
Clinical History, Part 3 (click here)
Clinical History, Part 4 (click here)
300-1. What is the differential diagnosis?
ANSWER
CASE NUMBER 503
(no virtual slide for this case)
Clinical History: A mother brought her 3-month-old infant to the pediatrician because the child had been alternately crying inconsolably or lying down listlessly; vomiting for the last 3 days, and had a mild fever. Physical exam reveals cherry red maculas. CSF analysis shows elevated protein levels. Gene sequencing reveals a mutation in the alpha-subunit of hexosaminidase A.
Image Gallery:
503-1. What is the differential diagnosis?
ANSWER
503-2. This disease is classified as which of the following?
- Glycogenosis
- Mucopolylipidosis
- Mucopolysaccharidosis
- Sphingolipidosis
- Sulfatidosis
ANSWER
503-3. Which of the following is true regarding this disease?
- Boys are affected more commonly than girls
- Most patients recover full neurological function in their teens
- The “cherry red macula” is due to retinal hemangiomas
- There is an increased incidence in Ashknazi Jews
- These patients are at increased risk for colon cancer
ANSWER
NERVOUS SYSTEM PATHOLOGY Review Items
Key Vocabulary Terms (click here to search any additional terms on Stedman's Online Medical Dictionary)
LEARNING OBJECTIVES
- Absolutely critical information you must know to practice medicine is in bold font.
- Important information that will be needed for routine patient care is in regular font.
- Information about less common diseases that you may encounter in clinical practice and that will probably appear on examinations is in italics
- Describe the morphology and function of the following CNS cells:
|
|
|
- choroid plexus epithelial cells
|
|
|
|
|
- Compare CNS myelin with PNS myelin, in terms of:
- cells of elaboration
- structure and function
- reactions to injury and destruction
- regenerative potential
- Discuss normal CSF in terms of:
- sites of formation
- circulation patterns
- sites of absorption
- pressure
- glucose and protein levels
- cell types present
- Describe the blood-brain barrier (BBB) in terms of:
- physiologic definition
- anatomic counterparts
- morphologic alterations
- areas of absence
- Describe the morphology and function of the following CNS cells:
|
|
|
|
|
|
- ischemic neuronal necrosis
|
|
|
|
|
|
- Compare and contrast the following types of cerebral edema and their significance:
- cytotoxic
- vasogenic
- interstitial
- Compare and contrast the clinical findings and sequelae of herniation of the brain:
- subfalcine (cingulate gyrus)
- transtentorial (uncal)
- foraminal (tonsillar)
- Correlate destructive lesions in specific areas of the CNS with corresponding functional consequences.
- Compare and contrast:
- communicating hydrocephalus
- non-communicating hydrocephalus
- hydrocephalus ex vacuo
- Describe the following congenital abnormalities and their clinical phenotype:
|
- spina bifida/meningomyelocele
|
- Chiari type I malformation
|
|
- Chiari type II (Arnold-Chiari) malformation
|
|
- Dandy-Walker malformation
|
|
|
- agenesis of corpus callosum
|
|
|
|
|
- Compare and contrast genetics, clinical presentation and pathology of inborn errors of metabolism:
|
- spina bifida/meningomyelocele
|
- Chiari type I malformation
|
|
- Chiari type II (Arnold-Chiari) malformation
|
|
- Dandy-Walker malformation
|
|
|
- agenesis of corpus callosum
|
|
|
|
|
- Describe the effects of hypoxia/ischemia on the late gestational/perinatal brain, including the pathophysiologic mechanisms underlying the following:
|
|
- germinal matrix hemorrhage
|
|
- periventricular leukomalacia
|
|
- Discuss the clinical and pathologic features of the following processes:
- Compare and contrast the clinical and pathologic features of CNS aneurysms:
- saccular ("berry"
- atherosclerotic
- Charcot-Bouchard
- mycotic
- Compare and contrast the clinical and pathologic features of CNS vascular malformations:
- arteriovenous malformation
- cavernous angioma
- capillary telangiectasia
- List the ways in which hypertension may harm the brain.
- Compare and contrast the clinical and pathologic features of:
- hypertensive encephalopathy
- hypoxic encephalopathy
- multi infarct dementia
- Compare and contrast the clinical and pathologic features of CNS infarcts:
- nonhemorrhagic (pale, anemic)
- hemorrhagic (red)
- border zone (watershed)
- incomplete
- spinal cord
- Compare and contrast clinical presentations of infarcts in these vascular territories:
- middle cerebral
- vertebrobasilar
- internal carotid
- Describe the interrelationship between hypotension and watershed infarcts.
- Explain the basis of the reperfusion theory of causation of hemorrhagic cerebral infarcts.
- Compare and contrast the clinical and pathologic features:
- skull fracture
- parencymal brain injury
- vascular brain injury
- Compare and contrast open vs. closed head injury, complications and prognosis.
- Compare and contrast the clinical and pathologic features of the following entities:
- pyogenic meningitis
- tuberculous/mycobacterial meningoencephalitis
- viral meningoencephalitis
- fungal meningitis
- neurosyphilis
- neuroborreliosis (Lyme disease)
- rickettsial infection
- protozoal infection
- List the common bacterial agents of acute pyogenic meningitis, and the age group that each most frequently affects.
- Compare and contrast the clinical and pathologic features:
- brain abscess
- subdural empyema
- extradural abscess
- Compare and contrast the clinical and pathologic features of viral meningoencephalitis:
- arboviral encephalitides
- herpes simplex viral encephalitis
- varicella-zoster viral encephalitis
- cytomegalovirus (CMV) encephalitis
- poliomyelitis
- rabies
- human immunodeficiency virus (HIV) infections
- HIV meningoencephalitis (subacute encephalitis)
- vacuolar myelopathy
- progressive multifocal leukoencephalopathy (PML)
- subacute sclerosing panencephalitis (SSPE)
- Discuss the clinical and pathologic features of the following prion diseases:
- Creutzfeldt-Jakob disease (CJD)
- variant CJD (vCJD, "mad cow" disease)
- kuru
- scrapie
- Compare and contrast the clinical and pathologic features degenerative diseases:
|
- olivopontocerebellar atrophy
|
|
|
|
- spinocerebellar degeneration
|
- progressive supranuclear palsy
|
- amyotrophic lateral sclerosis (ALS)
|
- corticobasal degeneration
|
|
- striatonigral degeneration
|
|
|
|
- Describe multiple sclerosis (MS) in terms of:
- geographic distribution
- etiology
- age at onset
- distribution of lesions
- morphology
- clinical course
- Discuss the following nervous system disorders:
|
- carbon monoxide poisoning
|
- acute ethanol intoxication
|
|
|
- central pontine myelinolysis (CPM)
|
|
|
- Discuss the clinical and pathologic features of the following nutritional disorders:
- Wernicke encephalopathy
- Korsakoff psychosis
- neuropathic beriberi
- subacute combined degeneration
- Explain the concepts of benign vs. malignant neoplasms of the CNS.
- Compare and contrast the clinical, pathologic, epidemiologic and genetic features of the following CNS neoplasms:
- colloid cyst of third ventricle
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- malignant peripheral nerve sheath tumor
|
|
|
- Compare and contrast the clinical, pathologic and genetic features of the following phakomatoses:
|
|
|
|
|
- von Hippel-Lindau syndrome
|
- Discuss the clinical and pathologic features of the following disorders of the PNS:
|
|
|
|
|
- paraproteinemia-associated neuropathy
|
|
|
- AIDS-associated peripheral neuropathy
|
|
- hereditary motor & sensory neuropathy (HMSN)
|
|
- type I [Charcot-Marie-Tooth disease (CMT) 1]
|
|
- type III (Dejerine-Sottas disease)
|
|
|